Non-alcoholic fatty liver disease (NAFLD) isn’t just about having a little extra fat in your liver. It’s a silent, progressive condition that can lead to serious damage-scarring, cirrhosis, even liver cancer. In 2023, the FDA officially reclassified it as MASH (Metabolic Dysfunction-Associated Steatohepatitis), reflecting how closely it’s tied to metabolic health. About 14.9 million U.S. adults have MASH, and the number keeps climbing. The good news? The most effective treatment isn’t a magic pill. It’s weight loss. But not just any weight loss. The kind that actually reverses liver damage.
How Much Weight Do You Need to Lose?
You don’t need to lose 50 pounds to see results. Studies show that losing just 5% of your body weight reduces fat in the liver. That’s 10 pounds for someone who weighs 200. But if you want to reverse scarring, you need more: 10% or higher. A 2022 study from the American Association for the Study of Liver Diseases found that only 25% of people who hit that 10% goal kept it off long-term. That’s the real challenge-not losing it, but keeping it off.
Why does weight loss help? Fat in the liver isn’t just storage-it’s toxic. It triggers inflammation, damages liver cells, and leads to fibrosis. Losing weight reduces that fat, lowers inflammation, and can even repair scar tissue. The more weight you lose, the better your liver function gets. ALT levels (a liver enzyme) drop. Liver stiffness decreases. Blood sugar improves. It’s not just about looking better. It’s about saving your liver.
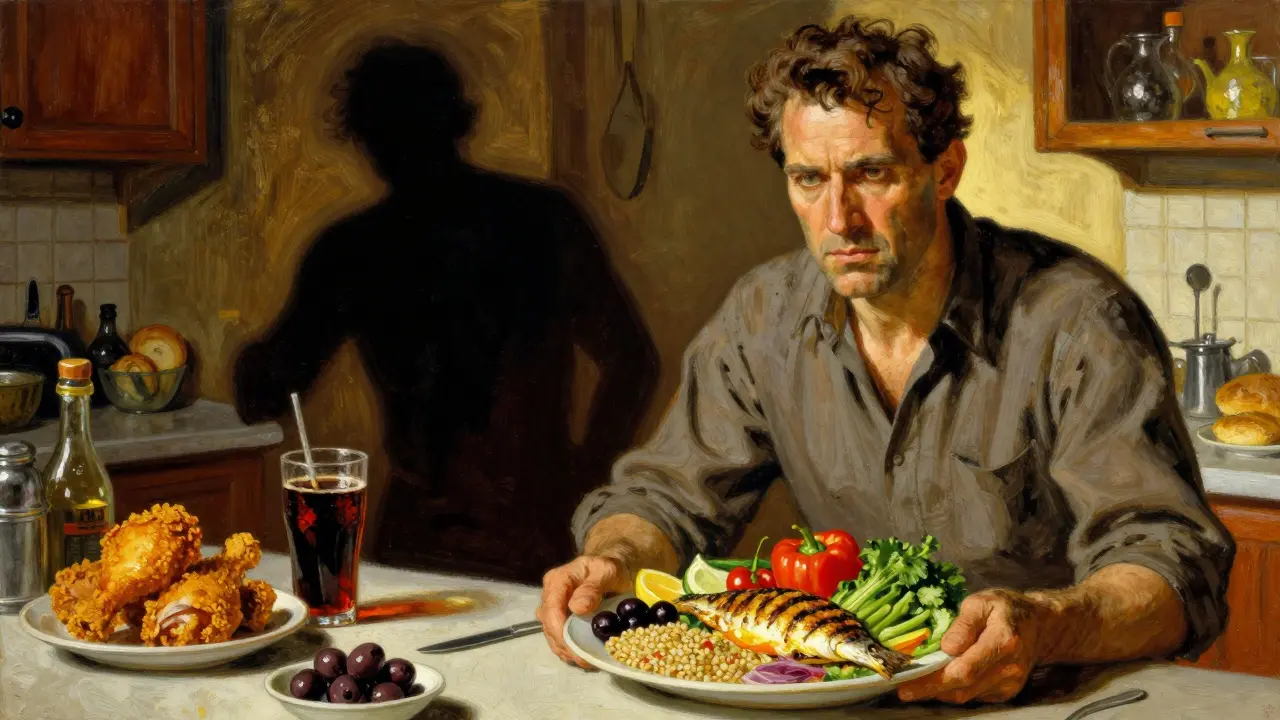
Diet: What You Should Actually Eat
Not all diets work for MASH. Crash diets? They backfire. Keto? May help short-term but isn’t sustainable. The best evidence points to one pattern: the Mediterranean diet.
This isn’t fancy. It’s simple. Load up on vegetables, fruits, whole grains, nuts, beans, olive oil, and fish. Cut back on sugar, refined carbs (white bread, pastries, soda), and saturated fats (fried foods, fatty meats). A meta-analysis showed this diet cut liver fat by 20%, lowered ALT levels, and reduced liver stiffness-all with statistical significance. People who followed it for a year saw measurable improvements in liver health, even without massive weight loss.
How many calories? Most people need a 500 to 1,000 calorie deficit daily to lose 1 to 2 pounds a week. That means swapping out a sugary breakfast for eggs and avocado, skipping the afternoon soda, and choosing a salad over fries. You don’t need to count every calorie, but you do need to be honest about portion sizes. A serving of pasta isn’t the whole box. A serving of nuts isn’t the whole bag.
And yes, alcohol is off-limits. Even small amounts can worsen liver damage. If you drink, stop. Full stop.
Exercise: Move More, Not Just Sweat
Exercise isn’t optional. It’s medicine. The Mayo Clinic recommends at least 150 minutes of moderate activity per week-that’s 30 minutes, five days a week. But here’s the twist: you don’t need to run a marathon. Brisk walking, cycling, swimming, even gardening counts.
Research shows that exercise alone-even without weight loss-can reduce liver fat. Why? It improves insulin sensitivity, lowers inflammation, and helps your body burn fat more efficiently. Add resistance training twice a week (bodyweight squats, dumbbells, resistance bands), and you boost muscle mass, which helps your metabolism work better long-term.
One study found that people who exercised regularly had less liver fat than those who didn’t, even if their weight stayed the same. Movement matters. Just moving more every day-taking the stairs, walking after meals, standing while you talk on the phone-adds up.

Medications: The New Game Changer
In August 2025, the FDA approved semaglutide (a GLP-1 receptor agonist marketed as Wegovy) for treating MASH in adults with moderate-to-advanced liver fibrosis. This was the first time a drug was approved specifically for liver damage caused by metabolic dysfunction. It’s a big deal.
Semaglutide works by mimicking a hormone that tells your brain you’re full. It slows digestion, reduces appetite, and helps control blood sugar. In clinical trials, nearly 90% of patients stayed on it for over a year. Two-thirds saw reduced liver inflammation. More than one-third saw actual improvement in liver scarring. Some had both.
But it’s not a magic bullet. It’s a tool. It works best when paired with diet and exercise. And it’s expensive-around $1,350 a month without insurance. Most insurance plans still don’t cover it for MASH, only for obesity or diabetes. That makes it inaccessible for many.
Other drugs? Metformin is cheap and widely used for type 2 diabetes, but studies show only modest benefits for the liver. Orlistat (a fat blocker) has weak evidence. SGLT2 inhibitors (like empagliflozin) are promising but still being studied. None have the same level of liver-specific data as semaglutide.
Here’s the catch: no medication has proven to be better than consistent lifestyle changes. If you lose 10% of your weight through diet and exercise, you’ll likely see better results than taking a drug without changing habits. Medications help when lifestyle alone isn’t enough.
What Works Best Together
The best outcomes come from combining all three: diet, exercise, and-if needed-medication.
- Diet: Mediterranean-style, low in sugar and refined carbs.
- Exercise: 150+ minutes of moderate activity weekly, plus strength training.
- Medication: Semaglutide for those with advanced fibrosis who’ve struggled with weight loss.
Doctors now see MASH as a metabolic disease-not just a liver problem. That means treating high blood pressure, high cholesterol, and insulin resistance alongside the liver. If you have diabetes, get your blood sugar under control. If you have high triglycerides, cut back on sugar and alcohol. Managing these pieces together gives you the best shot at reversing damage.
Real Challenges: Why People Struggle
Most people know what to do. But doing it? That’s harder.
Weight loss plateaus happen. Around 60% of people hit them after six months. Cravings return. Motivation fades. Stress triggers emotional eating. That’s normal. It doesn’t mean you’ve failed. It means you need support.
Work with a dietitian who understands liver disease. Join a weight-loss group. Use apps to track food and activity. Talk to your doctor about behavioral therapy. If you’ve tried before and failed, don’t give up. Ask for help. That’s what the Mayo Clinic says: “If you tried to lose weight in the past and couldn’t, ask your health care team for help.”
Semaglutide helps with appetite control, which is why so many stay on it. But side effects like nausea, constipation, or stomach cramps are common-especially at first. Most improve over time. If they don’t, talk to your doctor about adjusting the dose.
What’s Next?
The approval of semaglutide for MASH is a turning point. It proves that targeting metabolism can heal the liver. But it’s just the beginning. New drugs are coming-combination therapies, longer-acting versions, and drugs that directly target liver inflammation. Insurance coverage will improve. Costs will drop as generics enter the market.
For now, the foundation hasn’t changed. Lose weight. Move more. Eat real food. Avoid alcohol. And if you’re struggling, ask for help. Medications like semaglutide are tools-not replacements-for the hard work of changing your lifestyle. The liver is resilient. Give it a chance to heal, and it will.




Written by Martha Elena
I'm a pharmaceutical research writer focused on drug safety and pharmacology. I support formulary and pharmacovigilance teams with literature reviews and real‑world evidence analyses. In my off-hours, I write evidence-based articles on medication use, disease management, and dietary supplements. My goal is to turn complex research into clear, practical insights for everyday readers.
All posts: Martha Elena