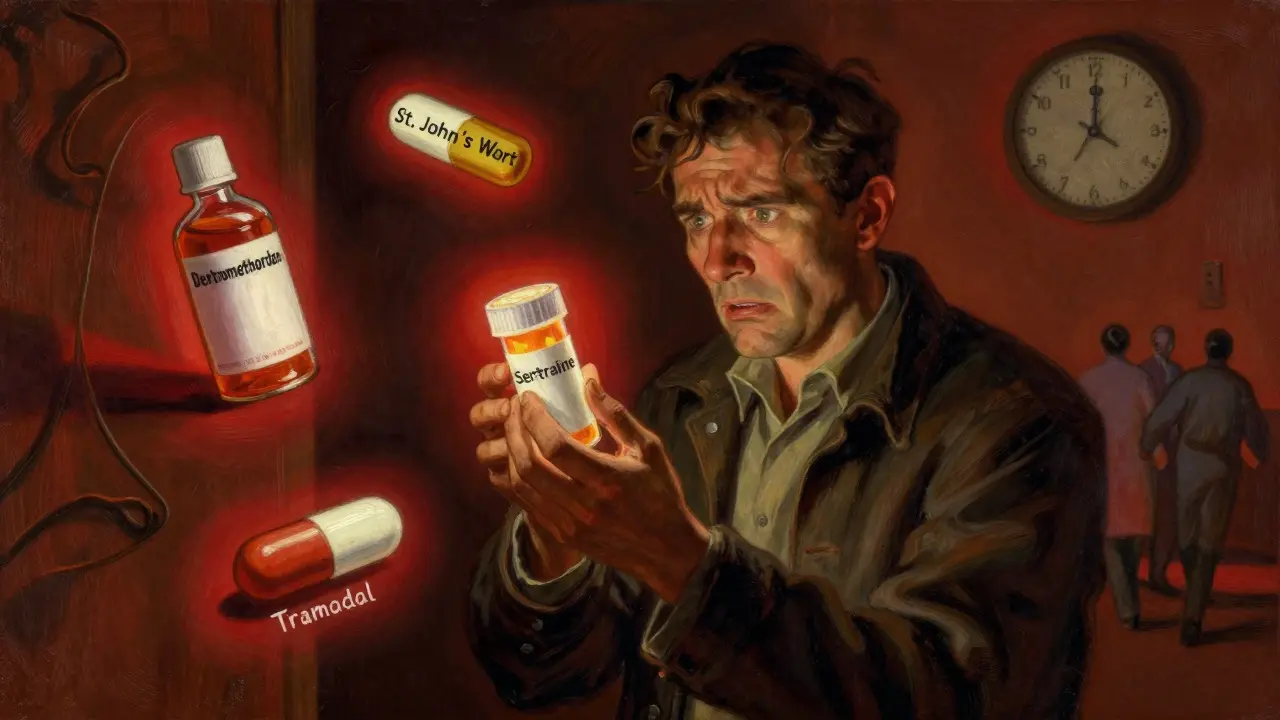
When you're taking an SSRI antidepressant like sertraline or escitalopram, you might assume it's safe as long as you don't miss a dose. But what you don't know could hurt you-especially if you're also taking another medication, supplement, or even an over-the-counter cough syrup. SSRI antidepressants are among the most prescribed drugs in the U.S., but their safety depends heavily on what else is in your system. The real danger isn't the SSRI alone-it's what it mixes with.
What Exactly Is Serotonin Syndrome?
Serotonin syndrome isn't a rare side effect you read about in fine print. It's a real, potentially deadly condition caused by too much serotonin in your brain. Think of serotonin as a chemical messenger that helps regulate mood, sleep, and muscle control. SSRIs stop your brain from reabsorbing serotonin, so more of it stays around. That's how they help with depression. But if another drug also boosts serotonin-like tramadol, St. John’s wort, or even some cold medicines-you can overload the system.The symptoms don’t sneak up slowly. They hit fast. You might feel suddenly shaky, sweaty, or feverish. Your muscles could lock up. You might have uncontrollable twitching, confusion, or a racing heart. In severe cases, your body temperature spikes past 104°F, your muscles go rigid, and you can slip into seizures or coma. It’s not anxiety. It’s not the flu. It’s serotonin syndrome-and it needs emergency care.
Which Medications Turn SSRIs Into a Time Bomb?
Not all drug combinations are equally risky. Some are outright dangerous. Others are just risky if you’re older, on multiple meds, or metabolize drugs slowly.High-risk combinations:
- MAOIs (like phenelzine or selegiline): Never take these with SSRIs. The risk of death is 30-50%. Even a two-week gap after stopping an SSRI isn’t enough if you’re on fluoxetine-wait five weeks.
- Linezolid (an antibiotic): Used for tough infections, but it blocks serotonin breakdown. A 2022 study found patients on SSRIs who took linezolid were nearly three times more likely to develop serotonin syndrome.
- Tramadol, dextromethorphan, and pethidine: These are common painkillers and cough meds. Tramadol alone increases serotonin syndrome risk by 4.7 times when paired with an SSRI. Dextromethorphan is in many OTC cough syrups. You might not realize you’re taking it.
Moderate-risk combinations:
- SNRIs (like venlafaxine or duloxetine): These work like SSRIs but also affect norepinephrine. Combining them with SSRIs raises serotonin syndrome risk more than threefold.
- Methadone and fentanyl: These opioids are often prescribed for chronic pain. They’re not as risky as tramadol, but they still double your chances of serotonin syndrome.
Low-risk opioids: Morphine, codeine, oxycodone, and buprenorphine show no significant increase in risk when taken with SSRIs. That’s why doctors now recommend switching from tramadol to oxycodone if you’re on an SSRI and need pain relief.
Herbs, Supplements, and OTC Drugs You Might Not Realize Are Dangerous
People think “natural” means safe. That’s a dangerous myth.- St. John’s wort: This herbal supplement for mild depression is a potent serotonin booster. One Reddit user reported uncontrollable shivering and confusion after just three days of mixing it with Prozac. The ER diagnosed early serotonin syndrome.
- Tryptophan and 5-HTP: Sold as sleep or mood aids, these directly increase serotonin levels. No doctor recommends combining them with SSRIs.
- Buspirone: Used for anxiety, it’s often prescribed alongside SSRIs-but it’s also a serotonin activator. The FDA explicitly warns against this combo.
- OTC cold and flu meds: Look for dextromethorphan on the label. Even one dose can trigger symptoms in someone already on an SSRI.
A 2022 GoodRx analysis found that 14% of people taking SSRIs with opioids reported mild symptoms like sweating and tremors-but only 2% went to the doctor. That’s a red flag. Many don’t know what they’re feeling is dangerous.

Who’s Most at Risk?
It’s not just about what you take-it’s who you are.- People over 65: Nearly 22% of Americans in this age group take SSRIs, and 18% use opioids. Many are on five or more medications. The body’s ability to clear drugs slows with age, making buildup more likely.
- People with CYP2D6 gene variants: This gene controls how your liver breaks down drugs like tramadol. If you’re a “poor metabolizer,” your body can’t process these drugs well. You’re 2.4 times more likely to develop serotonin syndrome.
- People recently starting or changing doses: The biggest spike in serotonin syndrome cases happens in the first few days after adding a new drug or increasing an SSRI dose.
One study found that 68% of serotonin syndrome reports in the FDA’s database involved drug combinations-not overdose. That means most cases aren’t from taking too much of one thing. They’re from mixing two things that seem harmless alone.
What Should You Do?
You don’t have to stop your SSRI. But you do need to be smart.- Know your meds: Keep a printed list of everything you take-prescription, OTC, supplements. Bring it to every doctor visit.
- Ask your pharmacist: Pharmacists are trained to catch dangerous interactions. A 2023 study showed pharmacist-led reviews cut serotonin syndrome events by 47% in Medicare patients.
- Watch for the 5 S’s: Shivering, Sweating, Stiffness, Seizures (rare), Sudden confusion. If you notice any of these after starting a new drug, go to the ER.
- Don’t self-medicate: No matter how mild your symptoms seem, don’t add St. John’s wort, 5-HTP, or cough syrup without checking with your doctor.
- Ask about alternatives: If you’re on an SSRI and need pain relief, ask if morphine or oxycodone is an option instead of tramadol. If you have anxiety, ask if buspirone is safe with your current meds.

What’s Changing in 2026?
The system is finally catching up.- By 2026, the FDA requires all electronic prescribing systems to show mandatory alerts when a doctor tries to prescribe an SSRI with tramadol, linezolid, or an MAOI.
- A new blood test called SerotoninQuant is in late-stage trials. It could one day confirm serotonin syndrome with a simple blood draw-something we don’t have now.
- The CDC now explicitly advises doctors to avoid tramadol, dextromethorphan, and pethidine in patients on SSRIs. This isn’t a suggestion-it’s a guideline.
These changes are good. But they won’t help you if you don’t speak up. You’re the last line of defense.
Real Stories, Real Consequences
One patient, 72, took sertraline for depression and tramadol for back pain. Within 12 hours of adding tramadol, he developed a 104.2°F fever, rigid muscles, and uncontrollable leg jerks. He spent three days in the ICU. His doctor had never asked if he was on any other meds. Another woman, 58, took Lexapro and St. John’s wort because she didn’t trust pharmaceuticals. After three days, she couldn’t think straight. She thought she was having a panic attack. The ER told her she had serotonin syndrome. She’s now off the herb and on therapy. These aren’t outliers. They’re examples of what happens when people assume their meds are safe to mix.Can you get serotonin syndrome from just one SSRI?
No, serotonin syndrome almost always happens when an SSRI is combined with another serotonergic drug. Taking a high dose of an SSRI alone rarely causes it. The real danger comes from mixing medications, supplements, or even OTC cough syrups.
How long does it take for serotonin syndrome to develop?
Symptoms usually appear within hours of taking a new drug or increasing a dose. In most cases, they start within 2 to 6 hours, but can take up to 24 hours. If you’ve just started a new medication and feel suddenly unwell, don’t wait.
Is serotonin syndrome permanent?
No, if caught early, serotonin syndrome is reversible. Stopping the offending drug and getting supportive care-like fluids and cooling-usually leads to full recovery within 24 to 72 hours. But if untreated, it can lead to organ failure or death.
Can I take melatonin with an SSRI?
Yes, melatonin is generally safe with SSRIs. It doesn’t significantly affect serotonin levels. However, always check with your doctor if you’re taking multiple supplements or have liver issues.
Why do some doctors still prescribe tramadol with SSRIs?
Some doctors aren’t aware of the updated guidelines, or they assume the patient isn’t taking other serotonergic drugs. Others believe the risk is low if the dose is small. But the data shows even low doses of tramadol with SSRIs can trigger serotonin syndrome. It’s not worth the gamble.
What should I do if I think I have serotonin syndrome?
Go to the emergency room immediately. Do not wait. Tell the staff you’re on an SSRI and recently started another medication. The sooner you get treatment, the better your outcome. Symptoms like high fever, muscle rigidity, or confusion are medical emergencies.





Written by Martha Elena
I'm a pharmaceutical research writer focused on drug safety and pharmacology. I support formulary and pharmacovigilance teams with literature reviews and real‑world evidence analyses. In my off-hours, I write evidence-based articles on medication use, disease management, and dietary supplements. My goal is to turn complex research into clear, practical insights for everyday readers.
All posts: Martha Elena