Medication Monitoring App Selector
Find Your Best Medication Monitoring App
Answer a few questions about your situation to get personalized recommendations for remote monitoring apps that help detect medication side effects.
Recommended Apps
Medisafe
Best for everyday use. Works with most wearables for real-time monitoring of heart rate, sleep patterns, and movement. Integrates with over 78 devices. Ideal for patients with 4+ medications and those who have a smartphone and wearable. Costs $99/year for healthcare providers.
AiCure
Best for high-risk clinical settings. Uses AI-powered video analysis to confirm medication ingestion and detect subtle signs of side effects. Requires $249/month per patient. Ideal for patients with multiple medications who need precise monitoring and are in clinical trials or under close supervision.
mySeniorCareHub
Best for elderly patients. Simple interface with voice prompts, large buttons, and caregiver alerts. Helps identify dangerous drug interactions before medication is given. Recommended for seniors taking multiple medications.
Note: These tools complement but don't replace your doctor. Always discuss alerts with your healthcare provider.
Every year, hundreds of thousands of people in the U.S. end up in the hospital because of unexpected reactions to their medications. These aren’t rare mistakes - they’re predictable, preventable events. The remote monitoring for medication side effects tools now available aren’t science fiction. They’re real, they’re working, and they’re changing how patients and doctors catch problems before they become emergencies.
How These Tools Actually Work
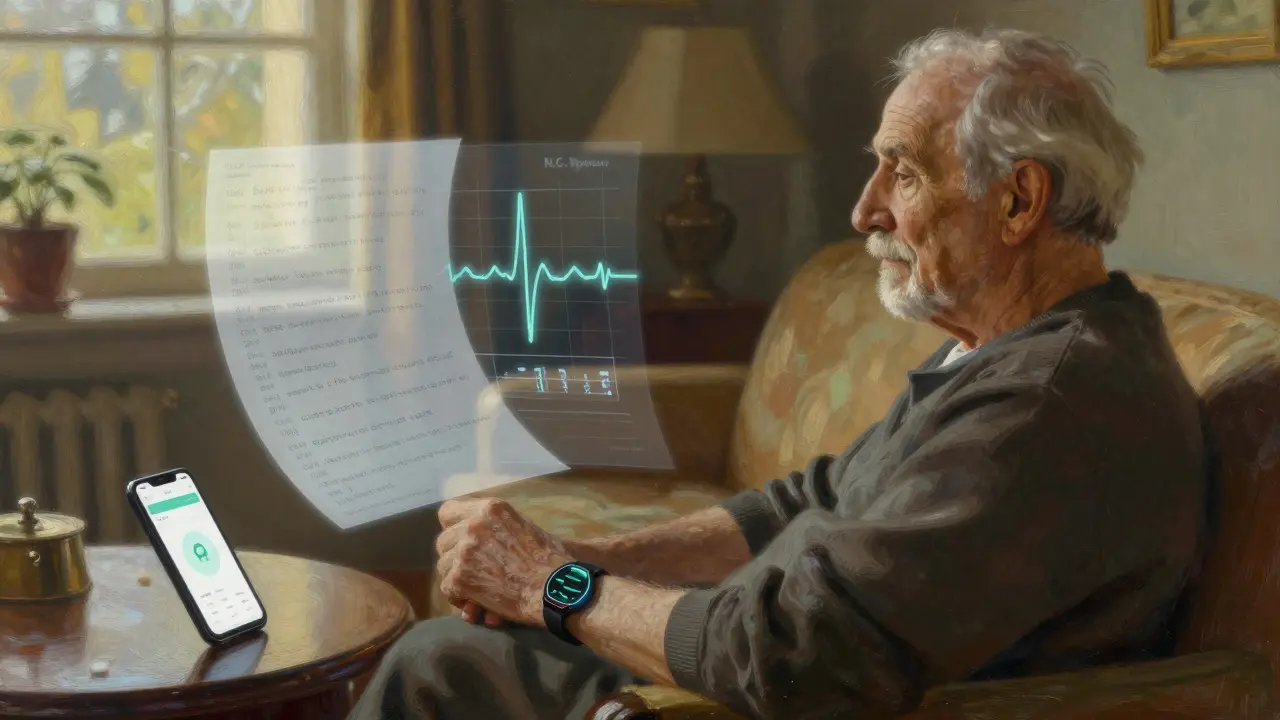
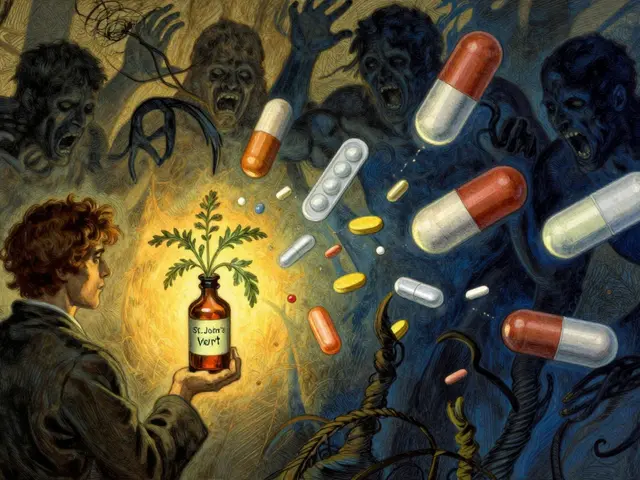
It’s not just about getting a reminder to take your pill. Modern systems track what you take, when you take it, and how your body responds - all in real time. Apps like Medisafe and AiCure don’t just send notifications. They connect to your Apple Watch, Fitbit, or other wearables to monitor heart rate, sleep patterns, and even subtle changes in movement. If your heart rate variability drops 15% over two days after starting a new blood pressure med, the system flags it. Not because it’s guessing - because it’s comparing your baseline to known patterns of side effects tied to that drug. AiCure uses your smartphone camera. It watches your face as you swallow a pill, confirms you took it, and then looks for signs of dizziness, slurred speech, or slowed movement. Its AI has been trained on over 2 million video samples. It’s 96.7% accurate at spotting when someone is experiencing side effects - not just forgetting their dose. Mango Health does something different. It listens. You type in how you’re feeling: "tired," "dizzy," "nauseous." Then it cross-references your symptoms with the FDA’s database of over 1.5 million reported adverse reactions. It doesn’t just match keywords - it understands context. If you’re on an antidepressant and report "fatigue," it knows that’s common. But if you report "fatigue + chest tightness + blurred vision," it sounds an alarm.What’s Actually Available - And What’s Not
Not all apps are built the same. Some are great at reminding you. Others are great at spotting problems. Few do both well. AiCure is the gold standard for clinical trials. Hospitals and pharma companies use it because it’s precise. But it costs $249 per patient per month. That’s not for everyday use. Medisafe, on the other hand, is designed for real life. It’s $99 a year for healthcare providers. It works with 78 wearables. It’s used by thousands of patients managing diabetes, heart failure, or depression. It doesn’t need a fancy camera. It just needs your watch to track your heart rate and your phone to log your pills. When the two don’t line up - say, your heart starts racing after taking a beta-blocker - it alerts your doctor before you even realize something’s wrong. Then there’s the Pill Identifier & Med Scanner app. It’s great if you’ve ever looked at a pill and wondered, "What is this?" It can identify over 15,000 medications with 94.6% accuracy using your phone’s camera. But it doesn’t track your vitals. It won’t warn you about drowsiness or liver stress. It’s a tool for verification, not prevention. HealthArc stands out for its depth. It pulls data from 42 different medical devices - glucose monitors, blood pressure cuffs, pulse oximeters - and uses its Adaptive Side Effect Detection Engine to find patterns across 1,850+ known medication-side effect links. But it’s complex. Clinicians need nearly 15 hours of training to use it well.The Big Problem: False Alarms
Here’s the catch: these systems aren’t perfect. They’re smart, but they’re not mind readers. And that’s where things get tricky. About 1 in 5 alerts is a false positive. That means if you’re on a medication that causes fatigue - like a beta-blocker or an antidepressant - the app might flag your normal tiredness as a side effect. One Reddit user said it made her anxious for weeks, thinking her medication was failing, when she was just having a bad week. Healthcare providers are feeling it too. In a survey by the American Medical Association, 68% said they’ve turned off alerts because they were too noisy. If you get 20 alerts a day and 18 are wrong, you stop paying attention. That’s dangerous. The real risk isn’t the tech. It’s the overconfidence in it. A patient might ignore a real symptom because "the app didn’t say anything." Or a doctor might miss a real issue because they’ve learned to ignore the system’s noise.
Who Benefits the Most?
This isn’t for everyone. But for some, it’s life-changing. Elderly patients on five or more medications? Huge win. The mySeniorCareHub app, launched in early 2025, flags dangerous drug interactions before a caregiver even gives the pill. Eighty-seven percent of users say it gives them peace of mind. People with chronic conditions like heart failure or diabetes? Also huge. At Mayo Clinic, AI monitoring cut severe drug reactions in their heart failure patients by 37%. How? By catching early signs of electrolyte imbalances from diuretics - before the patient felt dizzy or had a fall. But there’s a darker side. Early data from the Centers for Medicare & Medicaid Services shows these systems are less likely to flag side effects in elderly African American patients. Why? Because the AI was trained mostly on data from white, younger populations. The FDA now requires companies to test their algorithms across age, race, and gender groups - but that’s only been mandatory since February 2025. Many older systems still haven’t caught up.What’s Coming Next
The next leap isn’t just better sensors. It’s personalization. AiCure is testing something called "Digital Twin" technology. It builds a digital model of how your body reacts to drugs - based on your genetics, past reactions, and real-time data. In early trials, it improved side effect prediction by 43%. Imagine knowing before you even take a drug that it’s likely to make you dizzy - because your body’s history says so. The Mayo Clinic’s RIGHT Study is combining genetic testing with remote monitoring. They found that by identifying patients with specific gene variants, they could prevent 67% of adverse drug events before they started. That’s not just monitoring - that’s prevention at the DNA level. The FDA is also tightening rules. New guidelines for AI-based medical devices require stricter validation. That means fewer false alarms in the next 12-18 months. But it also means slower updates. Innovation will pause while companies retest.
What You Should Do Right Now
If you’re on multiple medications - especially for heart, mental health, or diabetes - ask your doctor: "Do you use any remote monitoring for side effects?" If they say no, ask if they’d consider it. Many clinics now get paid $52-$67 per patient per month through Medicare’s new Remote Therapeutic Monitoring codes. It’s financially viable for them. If you’re tech-savvy and have a smartwatch, try Medisafe. It’s free for patients, integrates with most wearables, and has a simple side effect log. Track your symptoms for a week. See if the app flags anything you didn’t notice. Don’t rely on it alone. But don’t ignore it either. These tools don’t replace your doctor. They give your doctor better eyes.Why This Matters More Than Ever
In 2024, adverse drug events cost the U.S. healthcare system $30 billion. That’s not just money. It’s lost time, broken bones from falls, emergency rooms filled with preventable crises, and families shaken by sudden hospitalizations. By 2027, experts predict these systems will prevent 1.2 million hospitalizations. That’s 1.2 million people who won’t have to spend a night in a hospital bed. 1.2 million families who won’t get the call at 2 a.m. The technology is here. The data is clear. The biggest barrier isn’t cost or capability. It’s awareness. Most patients don’t know this exists. Most doctors don’t know how to use it well. You don’t need to be a tech expert. You just need to ask the question: "Can we monitor this?" Because when it comes to your meds, seeing the unseen isn’t luxury. It’s safety.Can remote monitoring apps really detect medication side effects before I feel them?
Yes - in some cases. Apps like Medisafe and AiCure use wearable data (heart rate, movement, sleep) to spot subtle changes that happen before you notice symptoms. For example, a drop in heart rate variability can signal an adverse reaction to a beta-blocker 12-24 hours before dizziness or fatigue becomes obvious. These aren’t guesses. They’re patterns trained on clinical data from thousands of patients.
Are these apps safe for elderly patients who aren’t tech-savvy?
They can be, but only with support. Simpler apps like Medisafe and mySeniorCareHub are designed for older adults, with large buttons, voice prompts, and caregiver alerts. Cellular-enabled devices like Medtronic’s CareLink system work without Wi-Fi. The key is onboarding: having a nurse or family member help set it up. Patient engagement jumps from 63% to 89% when there’s hands-on support.
Do these apps replace visits to my doctor?
No. They enhance them. These tools give your doctor better data between appointments - like a continuous health log instead of a snapshot. But they can’t diagnose. If the app flags a possible reaction, you still need to talk to your provider. It’s like having a smart smoke alarm - it tells you something’s wrong, but you still need to check the kitchen.
What if the app gives me too many false alerts?
Alert fatigue is a real problem. If you’re getting too many non-critical alerts, talk to your provider about adjusting thresholds. Some systems let you mute alerts for specific symptoms (like fatigue) if they’re known side effects. You can also turn off non-essential features. The goal isn’t to be notified about everything - it’s to be notified about what matters.
Is my sensitive health data safe with these apps?
Most reputable apps are HIPAA-compliant and encrypt your data. But privacy concerns remain. Side effect data - like mood changes, dizziness, or heart rhythm issues - could be used by insurers to deny coverage if leaked. The FDA and HIPAA haven’t fully caught up with the risks. Ask your provider which app they recommend and review its privacy policy. Avoid apps that sell data to third parties.
Can I use these apps if I don’t have a smartphone or smartwatch?
Yes, but options are limited. Some systems use simple Bluetooth-enabled pill bottles that log when opened. Others use landline-based voice systems where you report symptoms by phone. But you lose the real-time physiological monitoring. For full benefits, you need a smartphone and a wearable. If you can’t use one, ask your clinic about low-tech alternatives like weekly check-in calls or paper symptom logs.
Are these apps covered by insurance?
In the U.S., Medicare now reimburses providers $52-$67 per patient per month for Remote Therapeutic Monitoring (RTM) that includes side effect tracking, as of late 2024. Many private insurers are following suit. But the coverage is for the provider’s service - not the app itself. You won’t get billed for the app, but your doctor must be enrolled in RTM to bill for it. Ask if your provider participates.
What’s the difference between Medisafe and AiCure?
Medisafe is designed for everyday use by patients and clinics. It’s affordable, integrates with consumer wearables, and focuses on adherence and symptom tracking. AiCure is built for clinical trials and high-risk populations. It uses AI-powered video analysis to confirm medication ingestion with 98% accuracy and detects subtle facial cues of side effects. But it’s expensive ($249/month) and requires more setup. Choose Medisafe for daily management. Choose AiCure only if you’re in a study or under close clinical supervision.




Written by Martha Elena
I'm a pharmaceutical research writer focused on drug safety and pharmacology. I support formulary and pharmacovigilance teams with literature reviews and real‑world evidence analyses. In my off-hours, I write evidence-based articles on medication use, disease management, and dietary supplements. My goal is to turn complex research into clear, practical insights for everyday readers.
All posts: Martha Elena