Most people don’t realize pancreatic cancer can be silent for months-until it’s too late. By the time symptoms show up, the cancer has often spread. That’s why survival rates stay stuck at just 12% for all stages combined. But here’s the thing: if caught early, before it spreads, the five-year survival rate jumps to 44%. The problem isn’t lack of progress-it’s missed signals. Early symptoms are vague, easily blamed on stress, aging, or digestive issues. And because there’s no routine screening for the general public, many don’t get tested until it’s advanced.
What Early Symptoms Are Often Overlooked?
Pancreatic cancer doesn’t scream for attention. It whispers. And those whispers get ignored.
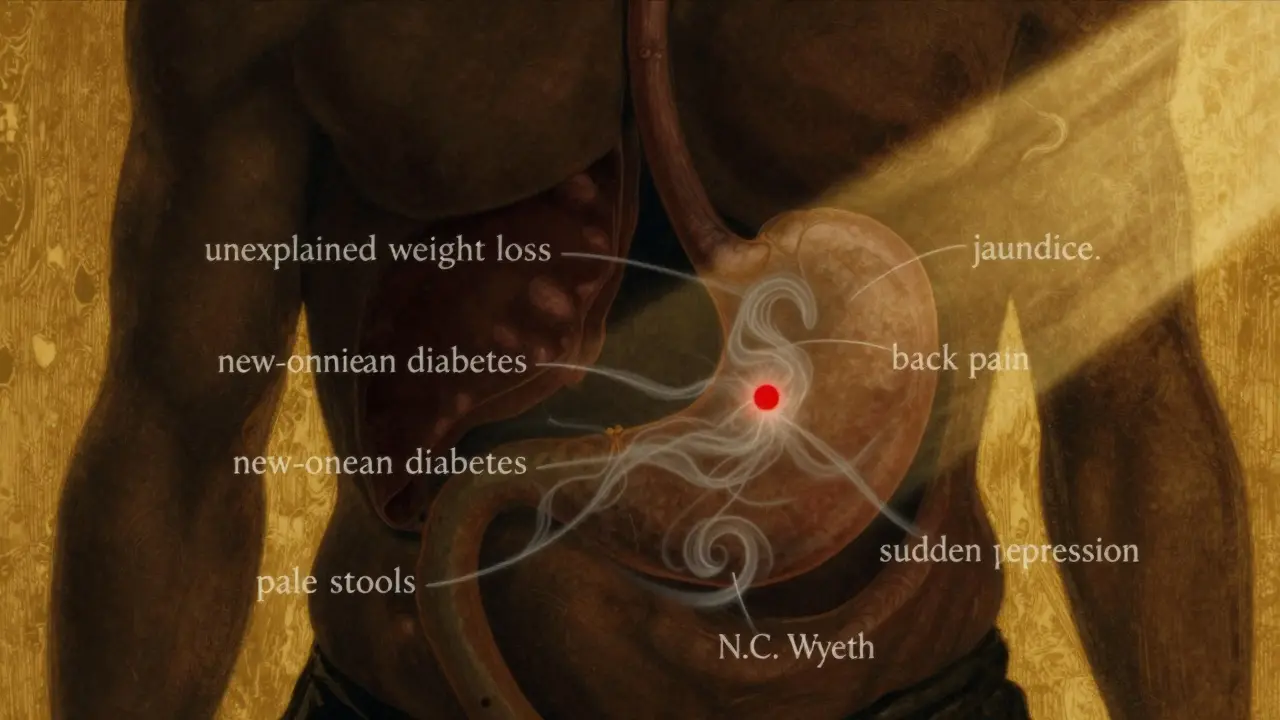
Unexplained weight loss is one of the most common red flags. People lose 10 pounds or more without trying-not from dieting, not from exercise. It just happens. Studies show about 60% of patients experience this before diagnosis. It’s not just about eating less. The pancreas stops making enough digestive enzymes, so food doesn’t break down properly. Calories vanish before the body can use them.
Then there’s jaundice. Yellow skin, yellow eyes, dark urine. This happens when a tumor blocks the bile duct. The liver can’t flush out bilirubin, so it builds up. About 70% of people with tumors in the head of the pancreas get jaundice. But here’s what many don’t know: severe itching often comes with it. Not just a little itch-constant, sleep-disrupting pruritus. It’s caused by bile salts building up under the skin. Many patients are misdiagnosed with eczema or allergies first.
New-onset diabetes is another hidden clue. If you’ve never had diabetes before, and suddenly your blood sugar spikes-especially if you’re under 50, not overweight, and not eating sugary foods-get tested. Research from Columbia University found that 80% of pancreatic cancer patients developed diabetes within 18 months before their cancer was found. Fasting glucose levels jump from normal (below 100 mg/dL) to diabetic levels (above 126 mg/dL) in just a few months. This isn’t coincidence. The tumor interferes with insulin production.
Back pain is another silent sign. Not the kind from lifting something heavy. This pain is deep, constant, and radiates from the middle of your back. It often gets worse after eating or when lying down. About two-thirds of patients report this. Many end up seeing chiropractors or getting MRIs for herniated discs-only to find the real issue is behind the stomach.
Changes in stool are easy to miss. If your poop is pale, greasy, and floats, it’s because fat isn’t being digested. The pancreas isn’t releasing enzymes. You might also notice nausea, loss of appetite, or bloating after meals. These are often written off as IBS or gallbladder problems. In fact, 72% of Reddit users with pancreatic cancer said they were first told they had gallstones or IBS.
And then there’s mood. Depression or anxiety that comes out of nowhere-no life event, no obvious cause. A 2018 study found that nearly half of pancreatic cancer patients had these psychiatric symptoms six months before physical signs appeared. Doctors rarely connect the dots. But the pancreas affects more than digestion. It’s tied to hormones, inflammation, and brain chemistry.
Why Is It So Hard to Diagnose Early?
The pancreas hides. It’s tucked behind the stomach, deep in the abdomen. You can’t feel a tumor during a regular exam. No stethoscope picks it up. No blood test alone confirms it.
CA 19-9 is the most common blood marker used, but it’s flawed. It only shows up in advanced cases. For early-stage cancer, it misses more than half the time. Imaging helps, but CT scans need tumors bigger than 2 cm to show clearly. Smaller tumors? Invisible.
That’s why diagnosis often takes months. Patients see three or four doctors. They get prescriptions for acid reflux, antidepressants, or painkillers. The average delay between first symptom and diagnosis is 4.2 months. By then, the cancer has often moved beyond the pancreas.
Screening doesn’t exist for the average person. But if you have a family history of pancreatic cancer, or carry a BRCA gene mutation, or have hereditary pancreatitis, you should be screened. High-risk individuals get annual MRIs and endoscopic ultrasounds. Johns Hopkins has been doing this since 2010-and their early detection rates are rising.
What’s Changed in Treatment?
Treatment used to mean one thing: surgery, if you were lucky enough to catch it early. But now, it’s a team effort.
The Whipple procedure-removing part of the pancreas, duodenum, and bile duct-is still the only chance for a cure. But only about 15-20% of patients are eligible at diagnosis. Still, for those who get it, five-year survival jumps to 20-25%.
Now, many patients get chemo before surgery. This is called neoadjuvant therapy. It shrinks tumors so they become operable. One combo, FOLFIRINOX (a mix of four chemo drugs), works wonders. In trials, it made 58% of borderline tumors shrink enough to be removed. And for those with metastatic disease, FOLFIRINOX doubled survival time-from 20 months to over 54 months.
Targeted therapies are changing the game too. If your tumor has a BRCA mutation, olaparib-a drug originally for breast cancer-can slow progression for nearly eight months longer than placebo. And if your cancer has MSI-H or dMMR markers (rare, but present in 3-4% of cases), pembrolizumab can trigger strong immune responses. Some patients see tumors shrink dramatically.
Even radiation has improved. New techniques like proton therapy deliver high doses with less damage to surrounding organs. This helps when surgery isn’t an option.
What’s on the Horizon?
The biggest hope isn’t a new drug-it’s early detection.
Johns Hopkins developed PancreaSeq, a blood test that finds DNA fragments from early-stage tumors. In high-risk groups, it’s 95% accurate. The DETECTA trial is testing a similar test that looks for protein markers and tumor DNA in blood. Early results show 85% accuracy.
AI is stepping in too. Google Health’s LYNA algorithm can spot cancer cells on pathology slides with 99.3% accuracy. That means pathologists can catch tiny signs faster. Microbiome research is also promising-scientists found that the gut bacteria in pancreatic cancer patients are different. A stool test might one day flag risk before symptoms appear.
And liquid biopsies? They’re coming fast. Dr. Diane Simeone at NYU says detecting mutant KRAS in blood could become routine within five years. That’s huge. KRAS mutations are in over 90% of pancreatic cancers. If we can find them early, we can act before the tumor grows.

Who Should Be Tested?
You don’t need to be scared. But if you have any of these, talk to your doctor:
- New-onset diabetes after age 50, especially without risk factors
- Unexplained weight loss with no clear cause
- Jaundice, dark urine, or pale stools
- Chronic back pain that doesn’t improve
- Depression or anxiety that started suddenly, with no life trigger
- Family history of pancreatic, breast, ovarian, or colon cancer
- Genetic mutation like BRCA1, BRCA2, Lynch syndrome, or PALB2
If you’re over 50 and have two or more of these symptoms, push for imaging. Don’t wait for a referral. Ask for a CT scan or MRI. If your doctor says it’s unlikely, ask why-and ask for a second opinion.
What Can You Do Now?
There’s no magic bullet. But awareness saves lives.
If you’ve had unexplained weight loss, new diabetes, or persistent back pain, write down your symptoms. Track when they started. Note any changes in appetite, stool, or mood. Bring this to your doctor. Don’t let them dismiss it as stress or aging.
If you have a family history, get genetic counseling. Even if you’re healthy, knowing your risk lets you start screening early. Programs at major cancer centers can monitor you for years before anything shows up.
And if you’re someone who’s been diagnosed-know this: survival is improving. Five years ago, metastatic pancreatic cancer meant months. Now, many live two, three, even five years with treatment. Clinical trials are open. New drugs are coming. You’re not alone.
Can pancreatic cancer be detected with a routine blood test?
No, there’s no routine blood test that catches early pancreatic cancer. The CA 19-9 marker is sometimes used, but it’s unreliable in early stages-it only detects about 30-50% of tumors before they spread. It’s more useful for tracking treatment response than for screening. New tests like PancreaSeq and liquid biopsies are promising but still in trials or limited to high-risk patients.
Is pancreatic cancer hereditary?
About 10% of pancreatic cancers are linked to inherited gene mutations. BRCA1, BRCA2, PALB2, Lynch syndrome, and hereditary pancreatitis are the most common. If you have two or more close relatives with pancreatic cancer-or a known genetic mutation-you should consider genetic testing and screening. Even if you don’t have symptoms, early monitoring can catch tumors before they spread.
Why does pancreatic cancer cause new-onset diabetes?
The pancreas makes insulin. When a tumor develops, especially in the head of the pancreas, it can damage the insulin-producing cells. This leads to high blood sugar-even in people who are thin and healthy. In fact, 80% of patients develop diabetes within 18 months before diagnosis. This isn’t just a side effect-it’s a warning sign. If you get diabetes after age 50 with no family history or obesity, ask your doctor about pancreatic screening.
Can you survive pancreatic cancer if it’s caught early?
Yes. If the cancer is caught before it spreads outside the pancreas, the five-year survival rate is 44%. Surgery-like the Whipple procedure-can remove the tumor completely. But only 15-20% of cases are caught this early. That’s why recognizing symptoms like jaundice, unexplained weight loss, and new diabetes is critical. Early detection saves lives.
What’s the most effective treatment today?
There’s no single best treatment-it depends on the stage and genetics. For early-stage, surgery followed by chemo is standard. For borderline or advanced cases, FOLFIRINOX chemo before surgery can shrink tumors enough to make removal possible. For metastatic cancer, FOLFIRINOX extends life to over four years in some patients. Targeted drugs like olaparib (for BRCA mutations) and pembrolizumab (for MSI-H tumors) offer hope for specific subtypes. Treatment is now personalized, not one-size-fits-all.
Are there any lifestyle changes that help prevent pancreatic cancer?
You can’t prevent it completely, but you can lower your risk. Smoking is the biggest avoidable factor-it doubles your risk. Quitting helps, even if you’ve smoked for years. Obesity and chronic pancreatitis also increase risk. Eating a diet rich in vegetables, avoiding processed meats, and staying active helps. But the biggest prevention tool is awareness: know your family history, pay attention to unusual symptoms, and don’t ignore new-onset diabetes or unexplained weight loss.




Written by Martha Elena
I'm a pharmaceutical research writer focused on drug safety and pharmacology. I support formulary and pharmacovigilance teams with literature reviews and real‑world evidence analyses. In my off-hours, I write evidence-based articles on medication use, disease management, and dietary supplements. My goal is to turn complex research into clear, practical insights for everyday readers.
All posts: Martha Elena