Elderly Medication Safety Checker
Check Medication Safety
Identify potentially risky medications for older adults based on the Beers Criteria. Enter medications you or a loved one is taking to see potential risks.
Safety Assessment
Older adults don’t just take more medications-they react to them differently. A pill that works fine for a 40-year-old might leave an 80-year-old dizzy, confused, or on the floor after a fall. This isn’t bad luck. It’s biology. As we age, our bodies change in ways that make medications more powerful, last longer, and sometimes turn harmful even at normal doses.
Why Older Bodies Handle Drugs Differently
Your liver and kidneys don’t work the same after 65. Blood flow to the liver drops by 30-40% between ages 25 and 75. That means drugs like diazepam or chlordiazepoxide-commonly prescribed for anxiety or sleep-stick around much longer. Instead of clearing in 24 hours, they can linger for days. That’s why an older person might feel groggy all day from a nighttime pill meant to help them sleep. Kidneys slow down too. After age 40, glomerular filtration rate (GFR) declines by about 0.8 mL/min/1.73m² every year. Drugs cleared by the kidneys-like digoxin, metformin, or certain antibiotics-build up in the bloodstream. Even a standard dose can become toxic. That’s why kidney function tests are non-negotiable before starting or adjusting meds in older adults. Body composition shifts too. Fat increases while muscle decreases. That changes how drugs are stored and released. Fat-soluble drugs like antidepressants or benzodiazepines get trapped in fat tissue and slowly leak back into the blood. This causes prolonged effects, sometimes long after the drug was supposed to wear off.The Silent Signs: What Side Effects Look Like in Seniors
In younger people, side effects are obvious: stomach upset, rash, headache. In older adults? They’re sneaky. - Falls: One in five falls in seniors is linked to medication. Dizziness from blood pressure pills, confusion from anticholinergics, or weakness from diuretics can all lead to a trip to the ER. - Confusion or memory lapses: Often mistaken for dementia, but could be a reaction to antihistamines, painkillers, or bladder medications. - Weight loss or appetite loss: Could be from antidepressants, NSAIDs, or even heart medications. - Low energy or depression-like symptoms: Sometimes just a side effect of beta-blockers, steroids, or proton pump inhibitors. These aren’t normal aging. They’re red flags. And they’re often missed because doctors and families assume it’s just “getting older.”Polypharmacy: The Hidden Danger
Taking five or more medications is called polypharmacy. It’s common-nearly 40% of adults over 65 take five or more drugs daily. But each extra pill multiplies the risk. Drug interactions aren’t just about two pills clashing. It’s about how multiple drugs overload the liver’s ability to process them. The CYP450 enzyme system, responsible for breaking down most medications, gets overwhelmed. One drug might slow down the breakdown of another, causing it to build up to dangerous levels. Some combinations are especially risky: - NSAIDs + blood thinners: Increases risk of bleeding ulcers by up to 15 times. - SSRIs + NSAIDs: Raises bleeding risk, especially in those with a history of falls or fractures. - Corticosteroids + NSAIDs: High chance of stomach bleeding. - Anticholinergics + benzodiazepines: Can cause severe confusion, urinary retention, and delirium. The more meds someone takes, the harder it is to know which one is causing the problem. That’s why medication reviews aren’t optional-they’re lifesaving.
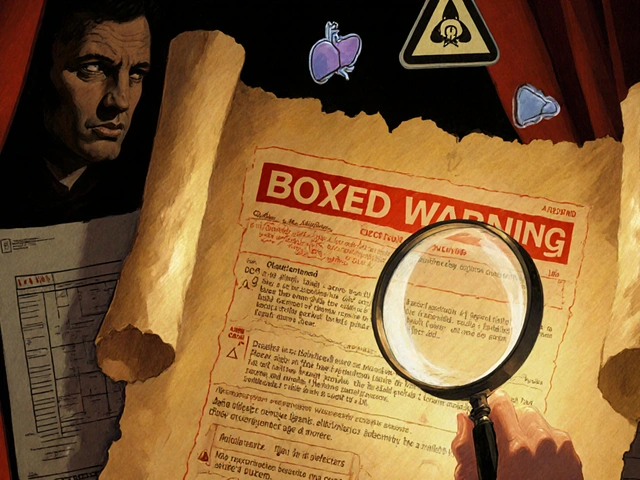
The Beers Criteria: A Lifesaving Tool
Since 1991, the Beers Criteria have been the gold standard for identifying medications that are risky for older adults. Updated in 2019 by the American Geriatrics Society, it lists drugs that should generally be avoided in people over 65-not because they’re useless, but because safer alternatives exist. Examples of drugs flagged in the Beers Criteria:- Glyburide: A diabetes drug that can cause dangerous low blood sugar in seniors. Safer options like glipizide or metformin are preferred.
- Meclizine: An antihistamine used for dizziness. Causes confusion and falls. Vestibular rehab is safer.
- Indomethacin: An NSAID with the highest rate of CNS side effects in older adults.
- Phenylbutazone: Rarely used now, but still on the list due to blood disorder risks.
- Sliding-scale insulin: Can lead to unpredictable lows. Basal insulin regimens are safer.
What to Do: Practical Steps for Safer Medication Use
If you or a loved one is over 65 and taking multiple medications, here’s what actually works:- Keep a full list: Include every prescription, OTC pill, vitamin, supplement, and herb. Don’t forget sleep aids, antacids, or cough syrup.
- Bring the list to every appointment: Not just your doctor-pharmacists, specialists, ER staff. Ask: “Could any of these be causing my dizziness or memory issues?”
- Ask about deprescribing: Don’t assume all meds are needed forever. Ask: “Is this still necessary? Can we try stopping it?”
- Watch for new symptoms: If you started a new drug and noticed confusion, falls, or loss of appetite, connect the dots. Tell your provider immediately.
- Use one pharmacy: That way, the pharmacist can check for interactions across all your meds.





Written by Martha Elena
I'm a pharmaceutical research writer focused on drug safety and pharmacology. I support formulary and pharmacovigilance teams with literature reviews and real‑world evidence analyses. In my off-hours, I write evidence-based articles on medication use, disease management, and dietary supplements. My goal is to turn complex research into clear, practical insights for everyday readers.
All posts: Martha Elena