FDA Drug Label Key Section Finder
Find Critical Information
Enter a drug name to see key sections from FDA drug labels. This tool helps identify warnings, dosing requirements, and approved indications.
Every pill you take, every injection you receive, comes with a story written in fine print. That story is the FDA drug label - not just a piece of paper in the box, but a legal, scientific, and life-saving document. If you’re a patient, caregiver, or even a healthcare provider, not knowing how to read it means you’re missing critical details about what the drug can and can’t do. And in a world where medication errors cause over 7,000 deaths annually in the U.S. alone, skipping this step isn’t just risky - it’s dangerous.
What You’re Really Looking At
The FDA drug label isn’t a brochure. It’s called the United States Prescribing Information (USPI), and it’s built to be read in layers. Think of it like a layered cake: the top layer is the Highlights, the middle is the Table of Contents, and the bottom - the biggest, densest part - is the Full Prescribing Information (FPI). The Highlights section is only half a page long, and by law, it must include a warning that it’s incomplete. That’s your first clue: never stop here.
The FPI contains 17 numbered sections, each with strict content rules. These aren’t suggestions - they’re requirements written into federal law (21 CFR 201.57). The FDA mandates this structure so that a doctor in New York, a pharmacist in Texas, and a nurse in Alaska all find the same critical information in the same place. It’s designed for speed and accuracy under pressure.
Section 1: Indications and Usage
This is where you find out what the drug is actually approved for. Not what your doctor thinks it might help with. Not what you read online. Only what the FDA has reviewed and approved based on clinical trials. For example, if a drug says it’s approved for "type 2 diabetes," that doesn’t mean it’s approved for weight loss - even if it causes weight loss as a side effect.
Look for the phrase "Established Pharmacologic Class" (EPC). This tells you how the drug works in the body - whether it’s a beta-blocker, a statin, a selective serotonin reuptake inhibitor (SSRI). Knowing this helps you understand why it’s being prescribed and how it might interact with other meds you’re taking.
Section 2: Dosage and Administration
This is the most commonly misread section. It doesn’t just say "take one pill daily." It tells you when to take it (with food? on an empty stomach?), how to take it (swallow whole? crush? dissolve?), and what to do if you miss a dose. But the real gold is in the modifications.
Look for dosing changes based on age, kidney function, liver problems, or weight. A 70-year-old with reduced kidney function might need half the dose of a healthy 30-year-old. If your doctor doesn’t adjust for this, you’re at risk for toxicity. The FDA updated guidance in March 2024 to require clearer language around these adjustments - so if you see vague terms like "use with caution," dig deeper into Section 8.
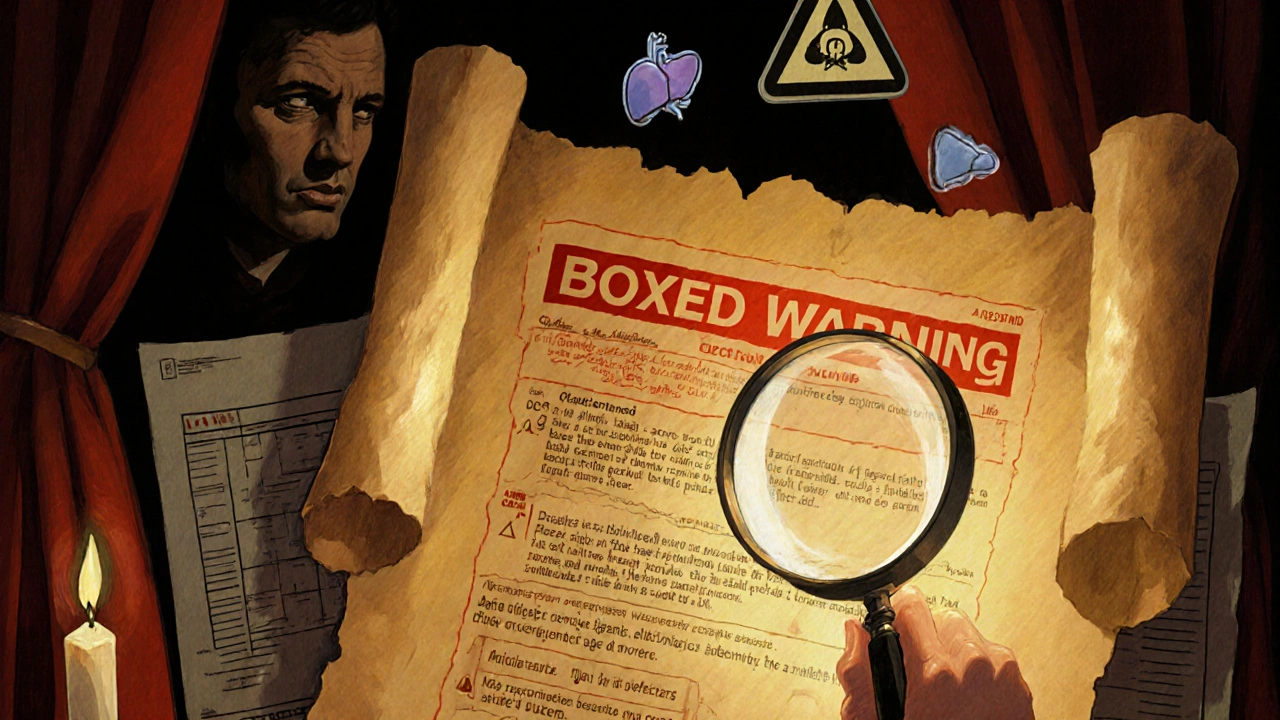
Section 5: Warnings and Precautions
This section contains the most important safety info - and it’s organized by severity. At the top? The Boxed Warning. It’s called that because it’s literally boxed in a thick border. This is the FDA’s highest alert. If a drug has a boxed warning, it means serious, sometimes fatal, risks have been proven - like liver failure, suicidal thoughts, or dangerous heart rhythms. No sugarcoating here. If you see this, you need to understand exactly what it means and what signs to watch for.
Below the box, you’ll find other warnings: risks of infection, bleeding, allergic reactions, or worsening of existing conditions. These aren’t "maybe" risks. They’re documented in clinical trials. If you have a history of heart disease, depression, or autoimmune disorders, this section tells you whether the drug could make it worse.
Section 6: Adverse Reactions
This is the side effect list - but not the kind you see on TV ads. Those ads only mention the most common ones. This list includes every reaction observed in clinical trials, ranked by frequency: very common (>10%), common (1-10%), uncommon (0.1-1%), rare (<0.1%).
Here’s what most people miss: if a side effect appears in this list at even 0.5%, it happened in real people during testing. That’s not a fluke. It’s data. If you’re taking a drug and feel something unusual - even if it seems minor - check this section. Is it listed? If yes, you’re not imagining it. If it’s not listed, that doesn’t mean it’s safe - just that it wasn’t seen in trials. But if it’s here, you need to know what to do.
Section 7: Drug Interactions
This section lists every medication, supplement, or food that can interfere with the drug. It’s not just about other pills. Grapefruit juice, St. John’s wort, even high-sodium diets can change how a drug works. The FDA requires this section to list interactions by severity: major, moderate, minor.
A major interaction means combining the two could cause serious harm - like sudden heart attack or kidney failure. A moderate one might reduce effectiveness or cause dizziness. Minor? Probably just a stomach upset. But if you’re on five or six medications, you’re playing Russian roulette unless you check this section. Pharmacists use this section daily to catch dangerous combos before they happen.
Section 8: Use in Specific Populations
Most drugs are tested on healthy adults in their 30s and 40s. But what about pregnant women? Kids? Elderly patients with multiple conditions? This section answers that. It breaks down safety and dosing by pregnancy category, breastfeeding status, pediatric use, and geriatric use.
For example, some drugs are labeled "not recommended in children under 12" because they weren’t tested. Others might be safe for elderly patients but only at lower doses. If you’re caring for someone outside the "average patient" profile, this section is your lifeline. Don’t assume your doctor knows all the data - read it yourself.
Section 16: How Supplied / Storage and Handling
Most people skip this. Big mistake. This section gives you the National Drug Code (NDC) - a 10-digit number that uniquely identifies the exact brand, strength, and packaging of your drug. If you’re switching pharmacies or getting a refill, this number ensures you get the same version. It also tells you how to store the drug: refrigerate? Keep in original bottle? Protect from light?
And here’s a hidden gem: it lists the manufacturer’s lot number. If there’s a recall, you can check if your batch is affected. In 2023, over 120 drug recalls were issued by the FDA - many because of contamination or incorrect dosing. Knowing your NDC could save your life.
Section 17: Patient Counseling Information
This section is written for you - not for doctors. It’s the FDA’s official script for what healthcare providers should tell patients about the drug. It includes plain-language advice: "Don’t drive until you know how this affects you," "Take with food to avoid nausea," "Do not stop suddenly."
Yet, only 38% of providers use it, according to a 2024 audit of 2,500 patient visits. Why? Time pressure. But you can use it yourself. Print it out. Read it before your next appointment. Ask your doctor: "Does this match what’s in Section 17?" If they’re not following the FDA’s own guidance, that’s a red flag.
The Hidden Section: Recent Major Changes
Since 2018, every label must include a "Recent Major Changes" section at the top. This tells you what’s been updated in the last six months. Maybe a new warning was added. Maybe the dosage changed. Maybe a dangerous interaction was discovered.
Drugs get updated constantly. A label from 2020 might be outdated. The FDA tracks that labeling updates happen every 14.3 months on average. If you’ve been taking a drug for years, check this section. It could explain why your doctor changed your dose or added a new test.
How to Use This in Real Life
Here’s how to read a label in under five minutes:
- Find the Boxed Warning - know the biggest risks.
- Check Section 1 - is this drug approved for your condition?
- Read Section 2 - how and when do you take it? Any adjustments for your health?
- Look at Section 7 - are any of your other meds or supplements listed?
- Flip to Section 17 - what should you be told about this drug?
- Check Recent Major Changes - has anything been updated since you started?
That’s it. You don’t need to memorize all 17 sections. Just know where to find the most critical info. And always, always cross-check with your pharmacist. They’re trained to spot what you might miss.
What Happens When You Don’t Read It
In 2023, the FDA issued 47 warning letters to drugmakers for labeling violations - meaning their labels were missing, wrong, or misleading. Patients paid the price. One case involved a blood thinner whose label failed to mention a key interaction with a common antibiotic. Patients developed internal bleeding. Another drug’s dosage instructions were printed incorrectly, leading to overdoses in elderly patients.
And it’s not just about mistakes. It’s about missed opportunities. A 2023 Johns Hopkins study found that when labels included clear, patient-friendly language, medication errors dropped by 29%. That’s not a small number. That’s lives saved.
The Future Is Changing
The FDA is testing new digital labels that let you click through levels of detail - basic info for patients, deep data for doctors. By 2027, most new drugs will come with this option. But for now, the printed label is still the law. And until the digital versions are mandatory, you still need to know how to read the old one.
Can I trust the Highlights section on a drug label?
No, not alone. The Highlights section is meant to be a quick snapshot, but by law, it must state that it’s incomplete. It leaves out critical details like dosing adjustments for kidney disease, rare but serious side effects, and drug interactions. Always read the Full Prescribing Information for the full picture.
What’s the difference between a Boxed Warning and other warnings?
A Boxed Warning is the FDA’s highest-level alert. It’s reserved for risks that are life-threatening or can cause permanent harm - like heart failure, severe liver damage, or suicidal behavior. Other warnings are important too, but they’re less severe. If a drug has a Boxed Warning, you need to understand it fully before taking it.
Why does the label list side effects that never happened to me?
Because those side effects happened to someone else in clinical trials. The label includes every reaction observed - even if it only affected 1 in 100 people. Just because you didn’t get it doesn’t mean it’s not real. It means you’re lucky. But if you start feeling something new, check the list. You might be one of the few.
How do I know if my drug’s label has been updated?
Look for the "Recent Major Changes" section at the top of the Full Prescribing Information. It lists every section that was updated in the last six months. If you’ve been taking the drug for more than a year, this section might explain why your doctor changed your dose or added a new test.
Can I use the Patient Counseling Information section to talk to my doctor?
Absolutely. Section 17 is the FDA’s official script for what your provider should tell you. If your doctor doesn’t mention the key points listed there - like avoiding alcohol or not stopping the drug suddenly - you can say, "This is what the FDA recommends patients be told. Can we go over this?" It puts you in control of your care.
Next Steps
Don’t wait for a crisis. Get the label for every prescription you’re taking. Go to the FDA’s website and search for the drug name - you’ll find the full prescribing information in PDF form. Print it. Highlight the Boxed Warning. Circle the dosing instructions. Write down the NDC number. Keep it in your wallet or phone.
If you’re helping someone else - a parent, an elderly relative - read the label with them. Ask questions. Don’t let them rely on a pharmacist’s quick summary or a Google search. This is their health. They deserve to understand it.
The FDA didn’t design this system to confuse you. It was built to protect you. But protection only works if you use it.



Written by Martha Elena
I'm a pharmaceutical research writer focused on drug safety and pharmacology. I support formulary and pharmacovigilance teams with literature reviews and real‑world evidence analyses. In my off-hours, I write evidence-based articles on medication use, disease management, and dietary supplements. My goal is to turn complex research into clear, practical insights for everyday readers.
All posts: Martha Elena