When you pick up a prescription, you might see two options: one with a familiar name like Lyrica or Viagra, and another with a long, unfamiliar chemical name. The brand-name version costs three, five, even ten times more. But here’s the thing - they’re basically the same drug. So why the huge price gap? And should you always pick the cheaper one?
The short answer: yes, you almost always should. Generic drugs aren’t second-rate. They’re not cheaper because they’re weaker. They’re cheaper because they don’t need to pay for ads, fancy packaging, or decades of research. And the data backs this up.
What Exactly Is a Generic Drug?
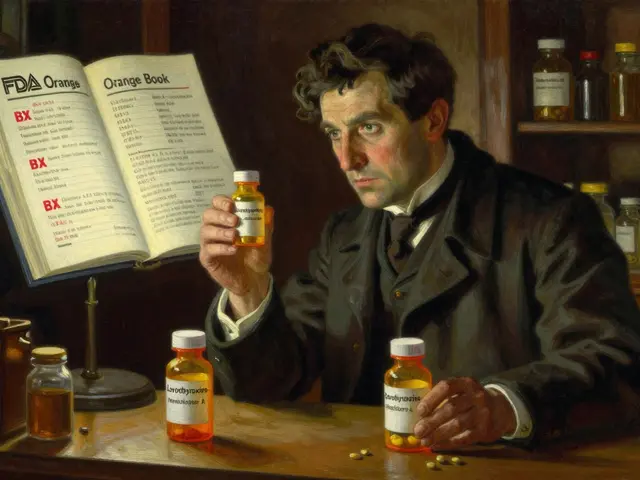
A generic drug contains the exact same active ingredient as the brand-name version. Same dose. Same way it’s taken - pill, injection, liquid. Same intended use. The FDA doesn’t just approve generics lightly. To get approval, a generic manufacturer must prove the drug delivers the same amount of medicine into your bloodstream at the same speed as the brand. That’s called bioequivalence. The standard? The generic’s performance must fall within 80% to 125% of the brand’s. That’s not a wide gap - it’s tight enough to guarantee the same effect.
Think of it like two brands of bottled water. One is Fiji. The other is a store brand. Same H₂O. Same minerals. Different label, different price. The generic is the store brand - same medicine, different packaging.
The system that made this possible started in 1984 with the Hatch-Waxman Act. Before then, companies had to repeat expensive clinical trials just to prove a generic worked. The law changed that. Now, they only need to prove they match the brand’s performance. That cut costs dramatically. And that’s why generics exist today.
The Real Price Difference
The numbers are shocking. In 2024, generics made up 90% of all prescriptions filled in the U.S. But they accounted for only 12% of total spending. Meanwhile, brand-name drugs, which made up just 10% of prescriptions, cost 88% of the money spent on prescriptions.
That means Americans spent $98 billion on 3.9 billion generic prescriptions. They spent $700 billion on 435 million brand prescriptions. That’s not a small difference. That’s a 79% to 85% price drop on average.
Here’s how it breaks down by competition:
- When only one generic enters the market, prices drop to about 90% of the brand’s original cost.
- With three to four generics, prices fall to 60%-70% of the brand’s price.
- When five or more generics are available, prices often drop below 50% of the brand’s original price.
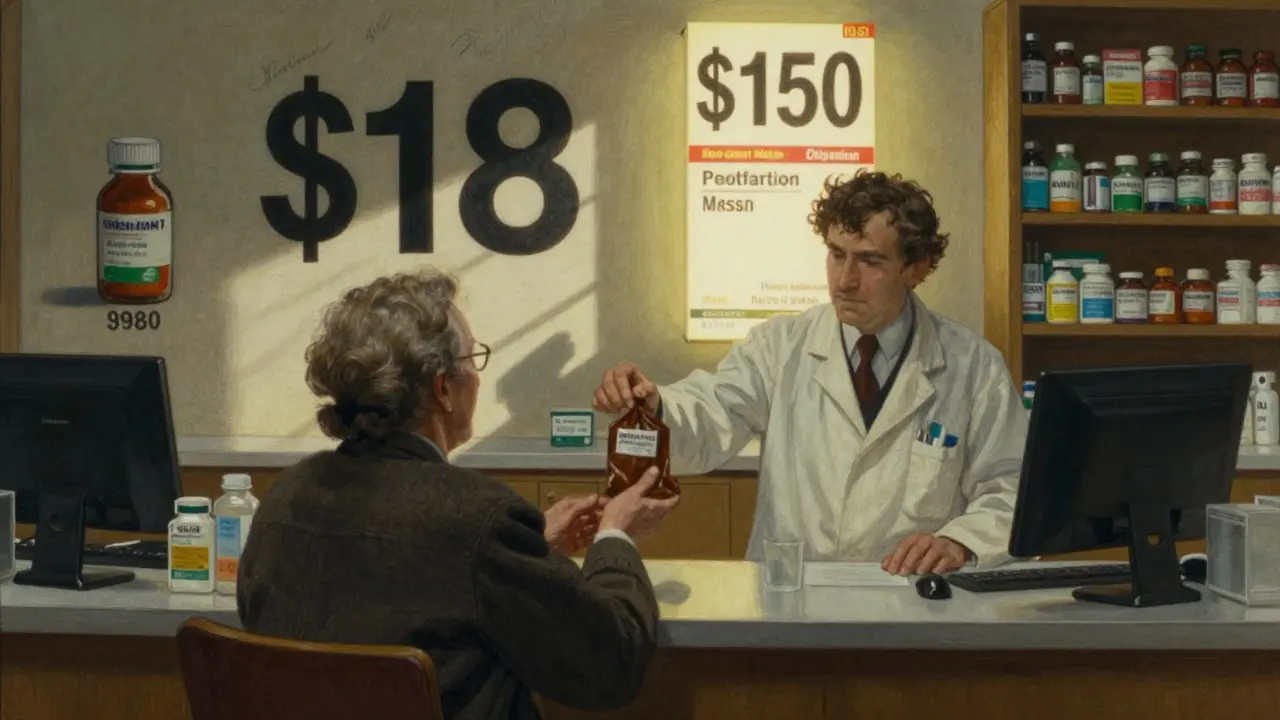
And it gets better over time. In markets with strong competition, prices keep falling. After three years, the average generic price drops another 20%. That’s why the same drug you paid $150 for five years ago might now cost $18.
Why Do Brand Names Cost So Much?
Brand-name drugs aren’t expensive because they’re better. They’re expensive because the company had to pay for research, clinical trials, marketing, and patent protection. Those costs are baked into the price - and they’re recouped before the patent expires.
Once the patent runs out, other companies can make the drug. They don’t need to repeat the expensive trials. They just need to prove they match the original. That’s why their costs are so low.
But here’s something most people don’t realize: brand-name companies are lowering their own prices too. When a generic is about to launch, some brands cut their prices to stay competitive. In 2025, Bayer cut the list price of Nexavar by 50% after its first generic version hit the market. Merck dropped Januvia’s price by 42.4%. Why? Because they knew the Medicare Inflation Reduction Act was coming - and it would force them to cut prices even more in January 2026.
So it’s not just generics driving prices down. Brand companies are playing the game too.
Are Generics Really Just as Good?
Yes. The FDA requires generics to meet the same strict standards as brand-name drugs. Same quality. Same purity. Same stability. Same effectiveness. The only differences are in inactive ingredients - things like dye, filler, or flavoring. These don’t affect how the drug works. They just change how the pill looks or tastes.
A 2025 survey of over 1,000 Americans found that 84% believe generics are just as effective. But 62% still trust brand-name drugs more. Why? Because of perception. Because of ads. Because they’ve seen the same logo for years.
But trust isn’t the same as science. The science says: generics work. The FDA says they work. Doctors say they work. And if you’ve ever taken a generic, you’ve probably already used one.
Why Do Some People Still Choose Brand?
Cost isn’t the only factor. In January 2025, 63% of Americans said they chose generics because they had to - not because they wanted to. Sixty percent said they’d prefer the brand if cost wasn’t an issue.
Some people worry about consistency. Maybe they had a bad experience once. Maybe their doctor told them to stick with the brand. Sometimes, especially with complex conditions like epilepsy or thyroid disease, doctors prefer to keep patients on the same formulation to avoid any possible variation.
But here’s the catch: even those cases are rare. For 95% of medications, switching to a generic is safe and effective. And if you do notice a difference? Talk to your pharmacist. Sometimes, switching to a different generic manufacturer can help. Not all generics are made by the same company.
What About Biosimilars?
You might hear the term biosimilar and think it’s the same as a generic. It’s not. Biosimilars are for complex drugs made from living cells - like biologics used for cancer, rheumatoid arthritis, or diabetes. They’re not exact copies like generics. But they’re very close. The FDA requires them to show no clinically meaningful difference from the original.
Biosimilars still cost less than the original biologic - often 15% to 35% less. And they’re becoming more common. As more biologics lose patent protection, biosimilars will become a major part of lowering drug costs.

What You Can Do Right Now
If you’re paying full price for a brand-name drug, ask your doctor or pharmacist: Is there a generic? If there is, ask why you’re not getting it. If your insurance won’t cover the generic, ask if they can change the prescription.
Check your pharmacy’s price list. Sometimes, the generic isn’t even the cheapest option. Some stores offer $4 or $10 generic lists for common medications. You don’t need insurance to get them.
And if you’re on Medicare, remember: the new $2,000 out-of-pocket cap in 2025 means your costs will change. Generics will help you stay under that limit.
Myths vs Reality
- Myth: Generics are made in lower-quality factories. Reality: The same factories often make both brand and generic drugs. The FDA inspects them all the same way.
- Myth: Generics take longer to work. Reality: Bioequivalence studies prove they work at the same speed.
- Myth: Generics aren’t as safe. Reality: The FDA tracks adverse events for both. No significant difference.
- Myth: If it’s cheap, it must be weak. Reality: The price reflects production cost, not effectiveness.
Final Thought: The System Works - If You Use It
The U.S. healthcare system has a strange but effective model. Brand-name drugs are expensive, but they fund innovation. Generics are cheap, and they make care accessible. Together, they keep prescription costs 18% lower than in other wealthy countries - even though the U.S. has the highest brand-name prices.
That’s not an accident. It’s the result of policy, competition, and consumer choice. And if you’re paying more than you need to, you’re not using the system the way it was designed.
Generics aren’t a compromise. They’re the smart choice. And they’ve been saving Americans billions every year since the 1980s. It’s time more people started acting like it.
Are generic drugs really as effective as brand-name drugs?
Yes. The FDA requires generic drugs to have the same active ingredient, strength, dosage form, and route of administration as the brand-name version. They must also prove bioequivalence - meaning they deliver the same amount of medicine into your bloodstream at the same rate. Studies show no meaningful difference in effectiveness or safety between generics and brand-name drugs for the vast majority of medications.
Why do generic drugs cost so much less?
Generic manufacturers don’t need to repeat expensive clinical trials. Once a brand-name drug’s patent expires, other companies can produce the same medicine using the existing data. This cuts research and marketing costs dramatically. Competition among multiple generic makers also drives prices down further - sometimes by over 80% compared to the original brand.
Can I switch from a brand-name drug to a generic without my doctor’s permission?
In most cases, yes. Pharmacists can substitute a generic for a brand-name drug unless the prescription specifically says "Do Not Substitute" or "Dispense as Written." But it’s still a good idea to talk to your doctor first - especially if you have a condition like epilepsy, thyroid disease, or a complex chronic illness where small changes can matter.
Why do some generic drugs look different than the brand?
The active ingredient is identical, but the inactive ingredients - like dyes, fillers, or coatings - can vary. That’s why generics might have a different shape, color, or taste. These differences don’t affect how the drug works. They’re just for manufacturing or branding purposes. If you’re concerned about the appearance, ask your pharmacist.
What if I think the generic isn’t working as well?
If you feel a difference after switching, talk to your doctor. Sometimes, it’s a placebo effect. Other times, you may be reacting to an inactive ingredient. You can ask for a different generic manufacturer - not all generics are made by the same company. In rare cases, your doctor may recommend staying on the brand. But for most people, the issue isn’t the drug - it’s the change in routine.
Are biosimilars the same as generics?
No. Biosimilars are for complex drugs made from living cells - like biologics used for cancer or autoimmune diseases. They’re not exact copies, but they’re very similar and must show no clinically meaningful difference from the original. They’re cheaper than the brand, but not as dramatically low-priced as traditional generics. Biosimilars are becoming more common as patents expire on biologic drugs.
Can I save money by buying generics at discount pharmacies?
Yes. Many pharmacies - including Walmart, Costco, and CVS - offer $4 to $10 generic lists for common medications like blood pressure pills, statins, or antibiotics. You don’t need insurance to use these programs. Even if you have coverage, it’s worth comparing prices. Sometimes, the cash price is lower than your copay.
Why do brand-name drug prices sometimes drop after a generic launches?
Some brand manufacturers lower prices to stay competitive. When a generic enters the market, the brand loses most of its sales. To keep some market share - or to prepare for future price caps like the Medicare Inflation Reduction Act - companies may reduce their list prices. For example, Bayer cut Nexavar’s price by 50% after its first generic launched in 2022.




Written by Martha Elena
I'm a pharmaceutical research writer focused on drug safety and pharmacology. I support formulary and pharmacovigilance teams with literature reviews and real‑world evidence analyses. In my off-hours, I write evidence-based articles on medication use, disease management, and dietary supplements. My goal is to turn complex research into clear, practical insights for everyday readers.
All posts: Martha Elena