Every year, tens of thousands of people in developing nations die from medicines that look real but contain nothing but flour, chalk, or worse-poison. These aren’t rumors. They’re facts backed by the World Health Organization, Interpol, and countless field reports from hospitals in Nigeria, Kenya, and Bangladesh. The problem isn’t just about fraud. It’s about survival.
What Exactly Are Counterfeit Drugs?
Not all fake drugs are the same. The WHO draws a clear line between two types: substandard and falsified. Substandard drugs are real products that were made poorly-maybe they expired, got stored in heat, or were diluted during shipping. Falsified drugs are outright scams. They’re made to look like the real thing but have no active ingredient, the wrong dose, or toxic chemicals mixed in.
Think of it this way: a substandard malaria pill might be 50% effective because it lost potency. A falsified one might have zero medicine in it at all. And in some cases, it’s laced with antifreeze or heavy metals. In 2024, a study in the Greater Mekong Subregion found that nearly 36% of antimalarial drugs failed quality tests. In some border areas, more than half of the antimalarials sold were fake.
Why Is This Happening in Developing Nations?
It’s not because people are careless. It’s because the system is broken.
In many low-income countries, the public health system is underfunded. Pharmacies are scattered, supply chains are long, and regulators lack the tools to inspect every shipment. A single medicine can pass through five or more middlemen before it reaches a rural clinic. At each stop, someone has a chance to swap it out.
And then there’s the price. Legitimate antibiotics or heart medications can cost 300% to 500% more than their counterfeit versions. For families living on less than $2 a day, the choice isn’t between safe and unsafe-it’s between buying medicine or buying food. Many know they’re taking a risk. But when your child is burning up with fever and the nearest real pharmacy is 30 kilometers away, you take the pills on the street corner.
Meanwhile, criminal networks have turned pharmaceutical counterfeiting into a high-margin business. Interpol estimates that counterfeit drugs can bring up to 9,000% profit. Compare that to drug trafficking or arms dealing-fake pills are easier to move, harder to trace, and carry lighter penalties.
The Human Cost: More Than Just Numbers
Behind every statistic is a person.
In 2012, over 200 people in Lahore, Pakistan died after receiving counterfeit heart medication. The pills contained toxic levels of an ingredient meant for industrial use. In 2022, cancer patients across several African countries received fake chemotherapy drugs that contained no active ingredients. One mother in Nigeria told a WHO interviewer: “My brother took the malaria pills they sold him. He got worse. Then he died. The pharmacy didn’t even know they were fake.”
Children are hit hardest. The OECD estimates that 72,000 to 169,000 child deaths from pneumonia each year are linked to fake or substandard antibiotics. In sub-Saharan Africa, more than 116,000 people die annually from fake antimalarials. These aren’t abstract numbers. These are children who never got a chance.
And it’s not just about immediate death. Fake antibiotics that contain too little medicine don’t kill you-they make bacteria stronger. This is how drug-resistant superbugs spread. The WHO calls this one of the biggest threats to modern medicine. If we lose the ability to treat simple infections, even minor surgeries could become deadly.
How Do These Fake Pills Get Into the Market?
The supply chain is the weak link.
Most counterfeit drugs originate in China, which produces 78% of the high-quality fakes, according to Interpol. But distribution hubs have shifted to places like Bangladesh, Lebanon, and Türkiye. These countries aren’t necessarily making the pills-they’re shipping them in bulk to regional markets.
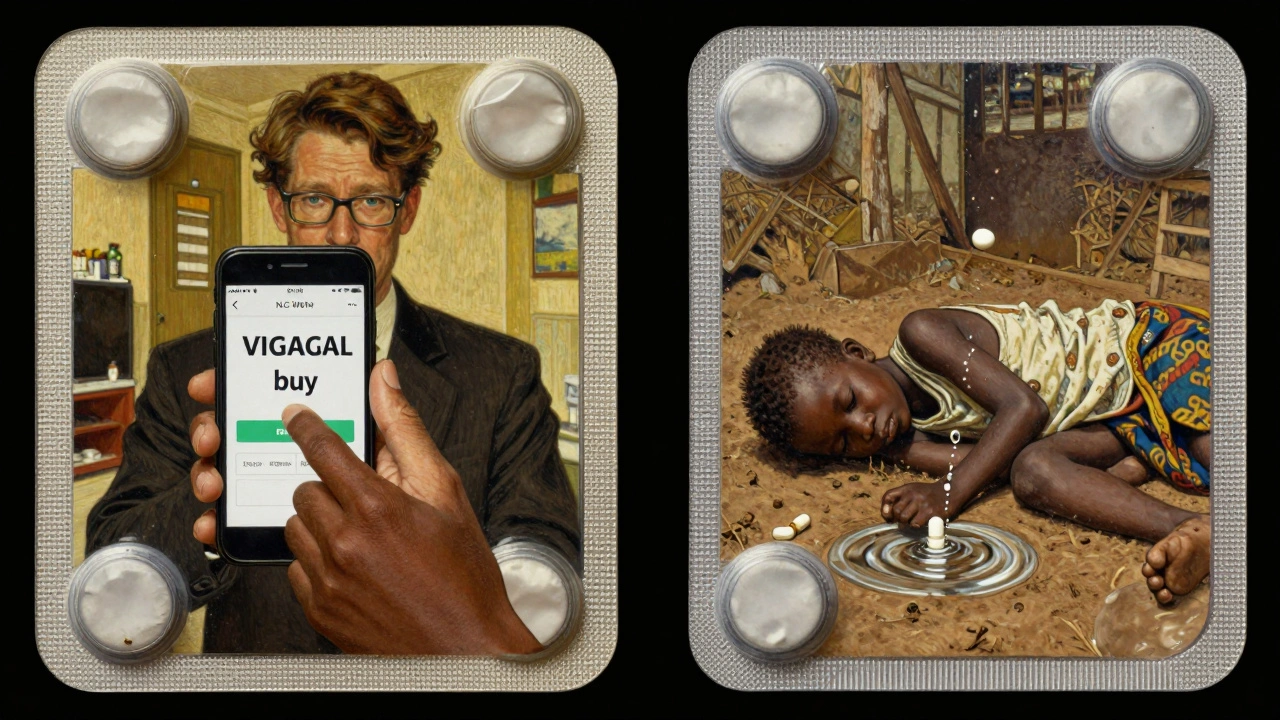
From there, the drugs enter local markets through informal networks: street vendors, unlicensed pharmacies, even mobile clinics. Online sales have made it worse. In Southeast Asia, 68% of negative reviews for online pharmacies mention suspected fake drugs. People buy pills from Facebook ads or WhatsApp groups, thinking they’re getting a discount. Instead, they’re getting death.
And the packaging? It’s terrifyingly good. Interpol says 90% of counterfeit medicines mimic real packaging with near-perfect accuracy. Even trained pharmacists can’t tell the difference by sight alone. Some fake pills now include holograms, QR codes, and even batch numbers that look legitimate. Criminals are using 3D printers to replicate blister packs down to the font size.
What’s Being Done to Stop It?
There are solutions-but they’re not reaching the people who need them most.
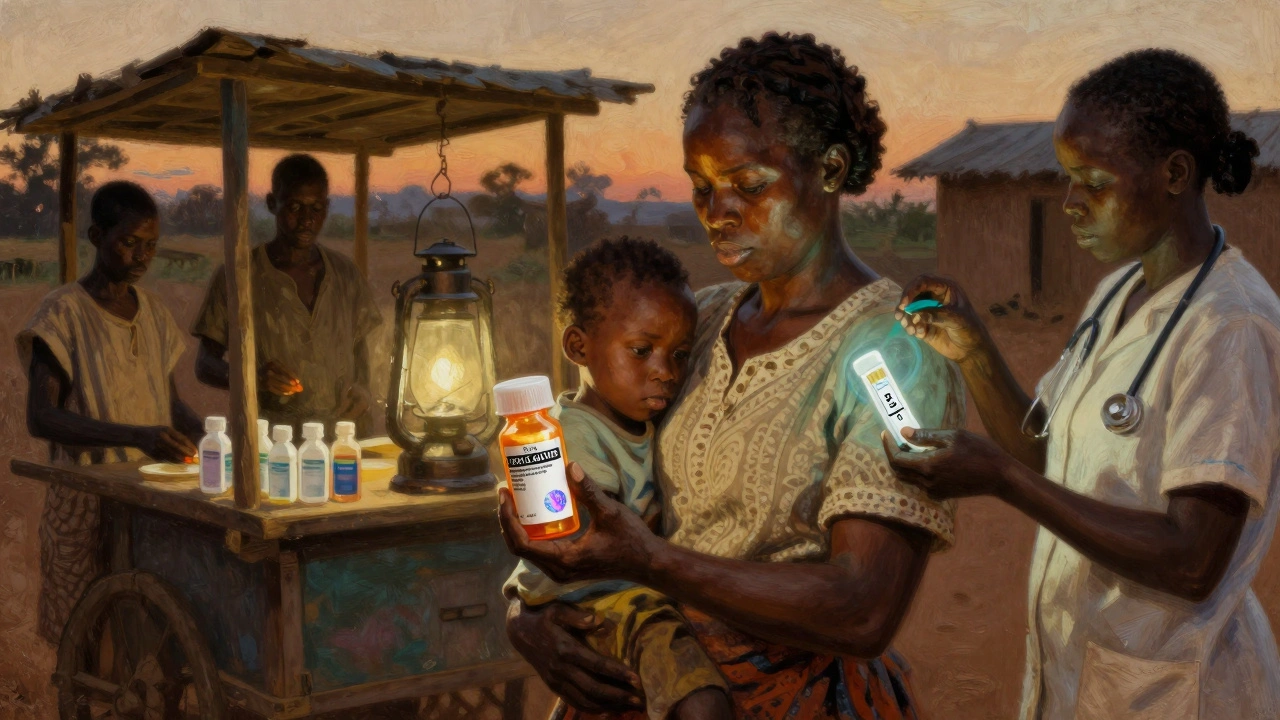
One promising tool is mPedigree, a system where users send a free SMS code from the medicine’s packaging to verify its authenticity. In Ghana, this system helped reduce counterfeit use by 37% in pilot areas. But here’s the catch: only 28% of users in low-literacy areas can use it without help. If you can’t read or don’t have a phone, the system doesn’t work.
Another solution is blockchain tracking. In March 2025, the WHO launched the Global Digital Health Verification Platform, which tracks medicines from factory to patient. So far, it’s active in 27 countries. But it only works if manufacturers, distributors, and pharmacies all plug in-and most rural clinics in Africa and South Asia still use paper records.
Some countries are trying to fix the system from the top. The EU has pledged €250 million to strengthen drug safety in 30 developing nations by 2026. The Medicrime Convention, signed by 76 countries, makes counterfeiting a criminal offense. But only 45 have turned it into actual law. Enforcement is still weak.
On the ground, community health workers are making a difference. In rural Kenya, volunteers are trained to spot red flags: unusual color, odd smell, packaging that feels cheap. They carry simple chemical test kits that cost $5 each and give 70% accuracy. It’s not perfect-but it’s better than nothing.

Why This Isn’t Just a “Developing Country Problem”
People assume this only happens far away. But counterfeit drugs are a global issue.
The U.S. FDA estimates only 1% of medicines in the U.S. are fake. That’s low-compared to 30% in some parts of Africa. But fake drugs still cross borders. A pill made in China might end up in a U.S. online pharmacy. A shipment meant for a clinic in Tanzania might get diverted through Dubai and sold in a European market.
And the same criminal networks that sell fake malaria pills in Nigeria also sell fake Viagra or weight-loss pills in the U.S. The tools are the same. The profit motive is the same. The only difference is who’s getting hurt.
What Can Be Done? Real Steps Forward
There’s no single fix. But here’s what works when it’s done right:
- Train community health workers to recognize fake drugs using simple tools-no lab needed. A 40-hour training program has reduced fake medicine use by over a third in pilot areas.
- Use solar-powered verification devices in clinics without electricity. These tools can test medicine quality in minutes and work even in remote areas.
- Expand SMS verification systems and make them voice-enabled for people who can’t read. In Ghana, a voice-based version increased usage by 60%.
- Hold online pharmacies accountable. Social media platforms and app stores must remove sellers of fake medicines-not just shut down websites, but track repeat offenders.
- Make real medicines affordable. Governments and NGOs need to negotiate lower prices for essential drugs. If the real medicine costs less than the fake one, people won’t take the risk.
The most important step? Stop treating this as a medical issue. It’s a criminal, economic, and human rights crisis. Until we treat it that way, people will keep dying.
What You Can Do
If you’re in a high-income country, you might think this doesn’t affect you. But it does. When fake drugs spread drug resistance, everyone loses. When people die from preventable diseases because of counterfeit pills, the entire global health system weakens.
Support organizations that work on medicine safety. Advocate for policies that fund drug verification in low-income countries. Don’t buy medicines from unverified online sellers-even if they’re cheap. And if you’re traveling, never buy pills from street vendors or unlicensed pharmacies.
This isn’t about charity. It’s about justice. Everyone deserves safe medicine-no matter where they live.
How common are counterfeit drugs in developing nations?
According to the World Health Organization, about 1 in 10 medicines in low- and middle-income countries are substandard or falsified. In some regions, like parts of Africa and Southeast Asia, the rate climbs to 30% or higher. For critical drugs like antimalarials, the rate can reach 50% in border areas.
Can you tell fake medicine apart from real medicine by looking at it?
It’s very hard. Counterfeiters now replicate packaging with 90% accuracy, including holograms, batch numbers, and even color variations. Even trained pharmacists can’t always tell the difference without testing. Some fake pills now use 3D printing to copy blister packs exactly.
What are the most common types of fake drugs?
Anti-infectives like antibiotics and antimalarials are the most common, making up 35% of counterfeit cases. Cardiovascular drugs (20%) and central nervous system medications (15%) are also heavily targeted. These are high-demand, high-profit drugs that people rely on daily.
Are fake drugs only sold on the black market?
No. Many fake drugs enter正规 pharmacies through corrupt supply chains. In some countries, even public hospitals have received counterfeit medicines. Online pharmacies, social media sellers, and mobile vendors are also major sources. The problem isn’t just illegal markets-it’s broken systems.
Is there a way to verify if a medicine is real?
Yes. Systems like mPedigree let you send an SMS code from the medicine’s packaging to check its authenticity. Some countries now use blockchain-based tracking, and simple chemical test kits cost as little as $5. But these tools aren’t widely available in rural areas due to lack of phones, electricity, or training.
Why don’t governments stop this?
Many lack the resources to monitor every shipment. Regulatory agencies are underfunded, understaffed, and often corrupt. Even when laws exist, enforcement is weak. In some places, the profit from fake drugs is higher than the salary of a health inspector. International cooperation is improving, but progress is slow.
What happens if you take a fake medicine?
It depends. If the pill has no active ingredient, your illness won’t improve-worse, it could get worse. If it has the wrong dose, you could overdose or underdose. Some contain toxic chemicals like antifreeze or industrial solvents, which can cause organ failure, seizures, or death. Long-term, fake antibiotics contribute to drug-resistant infections that are harder to treat.
Are there any success stories in fighting fake drugs?
Yes. Ghana’s mPedigree system reduced counterfeit medicine use by 37% in pilot areas. Rwanda and Senegal have improved drug tracking using mobile technology. In 2025, Interpol’s Operation Pangea XVI shut down 13,000 fake drug websites and arrested 769 suspects worldwide. These efforts show change is possible-but it needs funding, political will, and global cooperation.



Written by Martha Elena
I'm a pharmaceutical research writer focused on drug safety and pharmacology. I support formulary and pharmacovigilance teams with literature reviews and real‑world evidence analyses. In my off-hours, I write evidence-based articles on medication use, disease management, and dietary supplements. My goal is to turn complex research into clear, practical insights for everyday readers.
All posts: Martha Elena