When your skin starts flaking, red, and itchy, it’s easy to think it’s just dryness or eczema. But if you also notice your fingers or toes swelling up like sausages, or your lower back aches without any obvious injury, there’s a deeper issue at play. This isn’t just a skin problem - it’s an autoimmune storm affecting your whole body. Psoriatic arthritis is what happens when the same immune system that attacks your skin starts attacking your joints. And it’s more common than most people realize.
What Exactly Is Psoriatic Arthritis?
Psoriatic arthritis (PsA) isn’t just arthritis that shows up in people with psoriasis. It’s a distinct autoimmune condition where the body’s defense system turns on healthy tissue - both in the skin and the joints. About 30% of people with psoriasis will develop PsA, according to the American College of Rheumatology’s 2022 guidelines. In most cases, the skin comes first: about 85% of people notice scaly patches on their elbows, knees, or scalp before joint pain starts. But in 5-10% of cases, the joints hurt first, and the skin rash shows up later - which can make diagnosis tricky. The hallmark of PsA isn’t just swollen joints. It’s the combination of skin plaques, nail changes, and inflammation where tendons meet bone - called enthesitis. You might feel pain at the bottom of your foot or behind your heel, where the Achilles tendon connects. That’s not just soreness from walking too much. That’s your immune system firing off in the wrong place.How Do You Know If It’s PsA and Not Just Arthritis?
Not all joint pain is rheumatoid arthritis or osteoarthritis. PsA has its own fingerprint. One telltale sign is dactylitis - when an entire finger or toe swells up like a sausage. About 40% of people with PsA experience this. Another is nail pitting - tiny dents or ridges in your fingernails. Up to 80% of PsA patients have nail changes, which rarely happen in other types of arthritis. Doctors use the CASPAR criteria to diagnose PsA. It’s not one test. It’s a checklist: Do you have current or past psoriasis? Are your nails damaged? Is your rheumatoid factor negative (which rules out rheumatoid arthritis)? Do X-rays show bone changes like pencil-in-cup deformities? You get points for each. Score 3 or higher, and PsA is confirmed. The system is 99% specific - meaning if you meet the criteria, it’s almost certainly PsA. Blood tests for inflammation - like CRP and ESR - often come back high, but they’re not proof alone. Imaging matters. Ultrasounds and MRIs can spot early inflammation in tendons and joints before X-rays show damage. That’s why early diagnosis is so important. Once bone erosion starts, it’s often permanent.What’s Happening Inside Your Body?
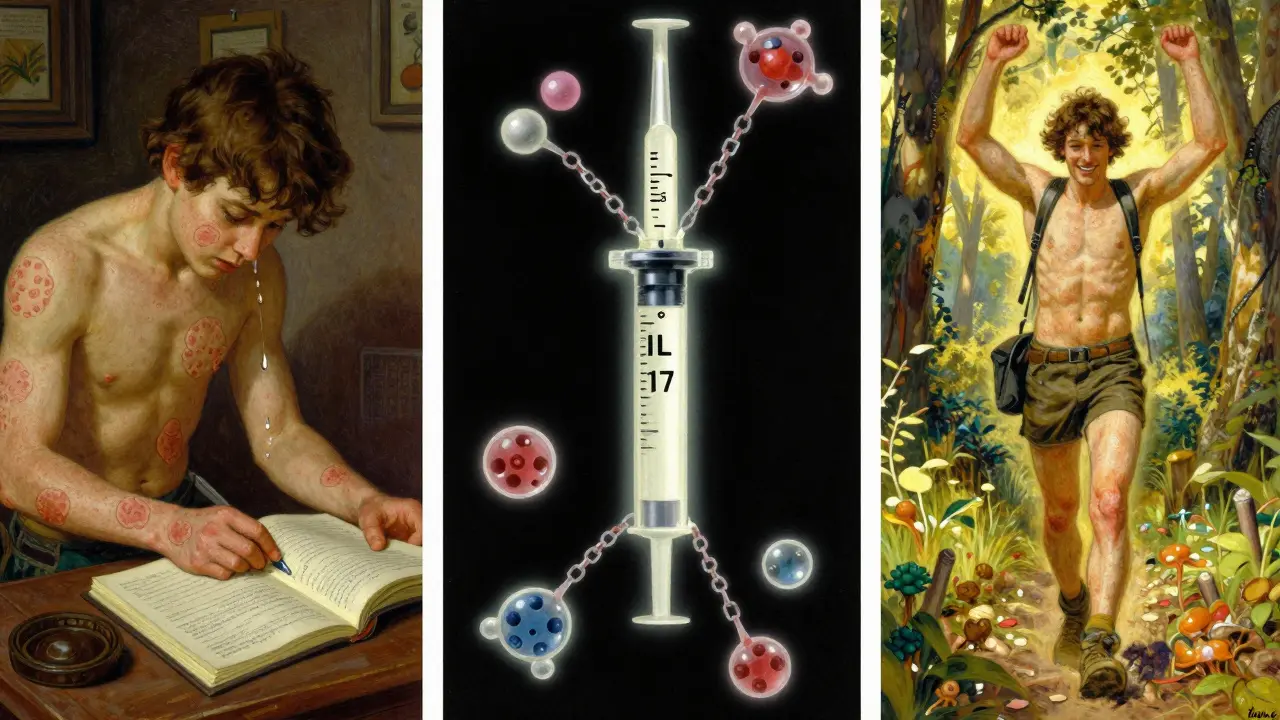
Your immune system is supposed to protect you. In PsA, it gets confused. It starts attacking your skin cells, making them grow too fast and pile up into thick, scaly plaques. Then it turns on the lining of your joints, causing swelling, pain, and stiffness. It also attacks the places where tendons and ligaments connect to bone - entheses - leading to chronic pain in the heels, hips, or spine. Genetics play a role. If you carry HLA-B27, HLA-B38, or HLA-B39 genes, your risk goes up. But genes alone don’t cause it. Triggers like stress, infections, injury, or even gut imbalances can flip the switch. Recent research shows PsA patients have different gut bacteria than people without the disease. That’s why some doctors now talk about the “gut-skin-joint axis” - a three-way connection that’s still being studied. The inflammation isn’t random. It’s driven by specific proteins: TNF-alpha, IL-17, IL-23. These are like alarm signals that keep your immune system fired up. That’s why treatments now target them directly.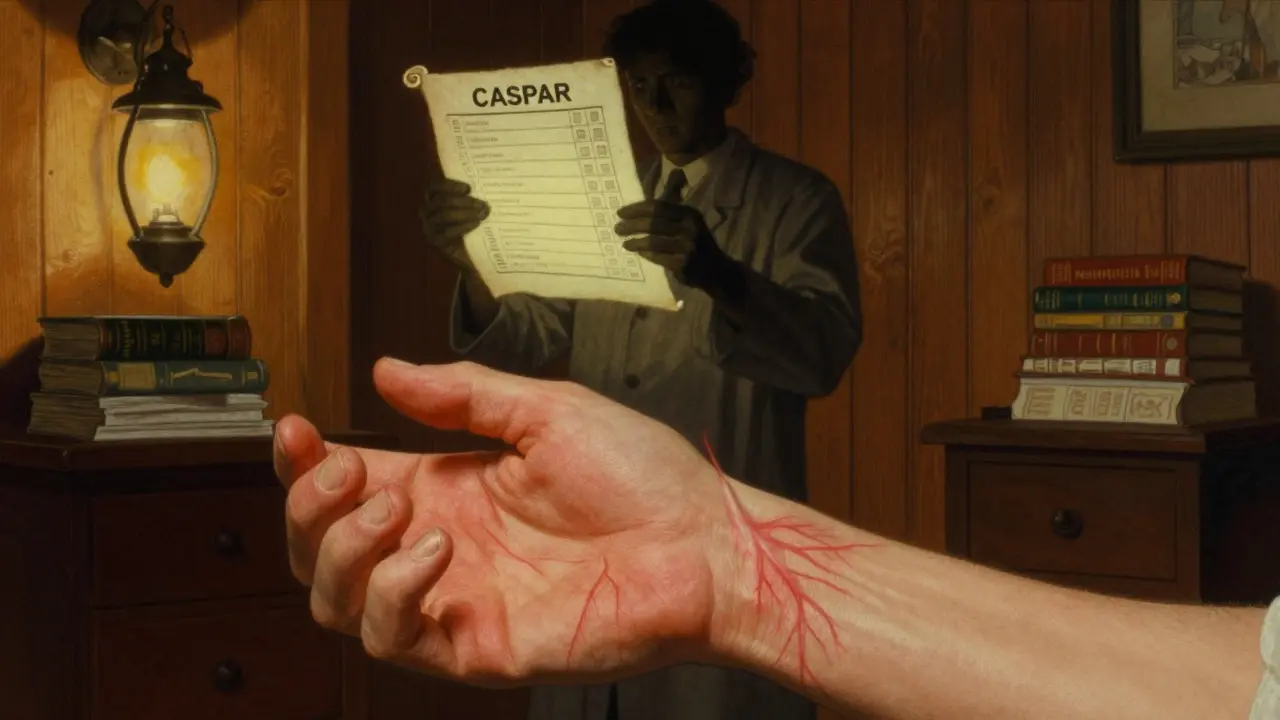
Treatment: From Pain Relief to Stopping the Damage
The goal isn’t just to feel better today. It’s to stop joint damage before it happens. That’s why treatment has shifted from simple painkillers to precision medicine. For mild cases, NSAIDs like ibuprofen help with pain and swelling. But they don’t change the disease. If symptoms stick around, doctors move to DMARDs like methotrexate. It slows the immune system down broadly, but it’s not always enough. For moderate to severe PsA, biologics are the game-changer. These are injectable or infused drugs that block specific inflammation signals:- TNF inhibitors (adalimumab, etanercept): Work well for joint and spine pain. About 50-60% of patients see a 20% improvement in symptoms.
- IL-17 inhibitors (secukinumab, ixekizumab): Better for skin plaques. Many patients report their skin clears up almost completely.
- IL-23 inhibitors (guselkumab, risankizumab): Newer options that target a different part of the inflammation chain. They’re showing strong results for both skin and joints.
- JAK inhibitors (tofacitinib, deucravacitinib): Oral pills that work inside cells. Good for people who don’t like injections.
What Does Success Look Like?
Success isn’t just “feeling better.” It’s reaching something called minimal disease activity (MDA). That means:- No more than 1 tender joint
- No more than 1 swollen joint
- Less than 1% of your skin covered in plaques
- Pain score under 15 out of 100
- Ability to do daily tasks without major struggle
- No constant fatigue
The Hidden Risks: More Than Just Skin and Joints
PsA doesn’t stop at your skin and joints. It’s a systemic disease. About half of people with PsA also have metabolic syndrome - high blood pressure, belly fat, insulin resistance, and bad cholesterol. That doubles your risk of heart attack. In fact, people with PsA have a 43% higher chance of having a heart attack than those without it. Depression and anxiety are common too. Nearly 1 in 3 people with PsA report feeling down or overwhelmed. That’s not just because of pain. Chronic inflammation affects brain chemistry. Studies show lower quality of life scores than people with diabetes or even some cancers. That’s why treatment now includes screening for heart disease, diabetes, and mental health. Your rheumatologist should ask about your mood, your sleep, your blood pressure - not just your swollen fingers.What’s Next? The Future of PsA Care
The next five years will change how PsA is managed. New drugs are coming fast. Bimekizumab, which blocks both IL-17A and IL-17F, is showing even better skin clearance than older drugs. Deucravacitinib, a new oral pill, targets a different pathway called TYK2 and has fewer side effects than older JAK inhibitors. Blood tests are getting smarter too. Doctors are starting to check for calprotectin and MMP-3 - proteins that signal how active the disease is. That could mean fewer scans and more precise treatment adjustments. By 2027, experts predict 70% of PsA patients will be on biologics or targeted pills within two years of diagnosis. That’s up from 40% today. Why? Because we now know: early, aggressive treatment saves joints, saves hearts, and saves lives.What You Can Do Right Now
If you have psoriasis and notice new joint pain, swelling, or stiffness - don’t wait. See a rheumatologist. Don’t assume it’s just aging or overuse. If your nails are pitted or your heel hurts without injury, that’s a red flag. Keep a symptom journal. Note which joints hurt, when, and how bad. Track your skin changes. Bring it to your doctor. The more detail you give, the faster you’ll get the right treatment. Lifestyle matters too. Losing even 5% of your body weight can reduce inflammation and improve drug response. Exercise - especially swimming or cycling - keeps joints mobile without pounding them. Quitting smoking cuts your risk of heart complications. And don’t ignore your mental health. If you’re feeling low, say something. There are support groups, therapists who specialize in chronic illness, and medications that help. Psoriatic arthritis is not a death sentence. It’s a manageable condition - but only if you act early. The right treatment can let you live without pain, without fear, and without limits.Can psoriasis turn into psoriatic arthritis?
Psoriasis doesn’t "turn into" psoriatic arthritis - they’re two parts of the same autoimmune condition. About 30% of people with psoriasis will develop joint symptoms, but not everyone does. The immune system is attacking both skin and joints at the same time, even if one shows up first. If you have psoriasis and notice new joint pain, swelling, or stiffness, it’s time to get checked.
Is psoriatic arthritis the same as rheumatoid arthritis?
No. Rheumatoid arthritis (RA) usually affects small joints symmetrically - like both wrists or both knees - and tests positive for rheumatoid factor. Psoriatic arthritis often affects joints unevenly, causes dactylitis (sausage fingers), and is linked to psoriasis and nail changes. RA doesn’t cause skin plaques. Blood tests and imaging help tell them apart, and treatment differs too.
Can psoriatic arthritis be cured?
There’s no cure yet, but it can be controlled. With the right treatment, many people reach minimal disease activity - meaning no pain, no swelling, and no skin plaques. The goal is to stop joint damage before it happens. Early treatment with biologics or targeted drugs can keep the disease in remission for years, sometimes decades.
Does psoriatic arthritis only affect the hands and feet?
No. While fingers and toes are common, PsA can affect any joint - including the spine, hips, shoulders, and even the jaw. About half of patients develop axial involvement, meaning inflammation in the spine or sacroiliac joints, which causes back pain. That’s why it’s sometimes mistaken for ankylosing spondylitis. A full assessment by a rheumatologist is needed to map all affected areas.
Are biologics safe for long-term use?
Biologics are generally safe when monitored. They suppress parts of the immune system, so there’s a slightly higher risk of infections like tuberculosis or fungal infections. That’s why doctors test for latent TB before starting treatment. Regular blood tests and check-ups catch issues early. For most people, the benefits - stopping joint damage, reducing pain, improving quality of life - far outweigh the risks.




Written by Martha Elena
I'm a pharmaceutical research writer focused on drug safety and pharmacology. I support formulary and pharmacovigilance teams with literature reviews and real‑world evidence analyses. In my off-hours, I write evidence-based articles on medication use, disease management, and dietary supplements. My goal is to turn complex research into clear, practical insights for everyday readers.
All posts: Martha Elena