Medication Lung Injury Risk Checker
Check if your current medications might be causing lung symptoms. This tool helps identify if a medication could be contributing to cough, breathlessness, or other respiratory issues.
Risk Assessment
Symptoms to watch for:
Next steps:
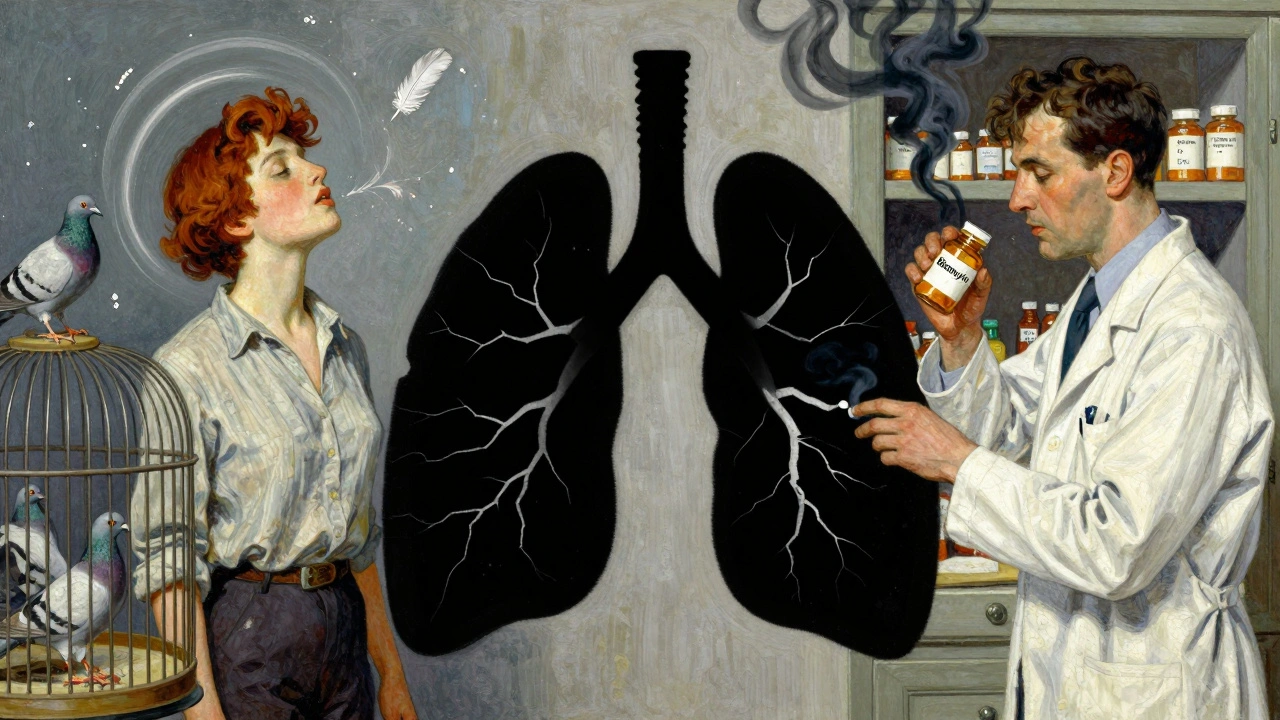
When you start coughing and can’t catch your breath, it’s easy to blame allergies, a cold, or even the weather. But if these symptoms don’t go away - and they get worse after taking a new medication - something more serious could be happening. Many people assume that if a drug causes lung trouble, it must be hypersensitivity pneumonitis. But here’s the truth: true hypersensitivity pneumonitis isn’t caused by pills or injections. It’s caused by breathing in tiny particles from the environment - mold, bird droppings, hay dust, or humidifier bacteria. Medications don’t trigger this specific immune reaction in the lungs.
What Actually Causes Hypersensitivity Pneumonitis?
Hypersensitivity pneumonitis (HP) is an immune response triggered when you inhale certain organic particles over time. Your body sees them as invaders and attacks, causing inflammation deep in the lung sacs - the alveoli. This isn’t asthma. It’s not bronchitis. It’s a distinct type of lung injury that shows up on scans as patchy ground-glass shadows and air trapping.
Common triggers include:
- Bird proteins (feathers, droppings) - known as bird fancier’s lung
- Moldy hay or grain - farmer’s lung
- Fungi from mushroom growing environments
- Bacteria in hot tubs or poorly cleaned air conditioners
People who work with these materials - farmers, bird breeders, mushroom harvesters, or even people with indoor water features - are at higher risk. Symptoms often appear hours after exposure: sudden fever, chills, cough, and shortness of breath. If you leave the environment, you feel better within a day or two. That’s a major clue.
But if you keep breathing in the trigger? Over months or years, the inflammation turns into scarring. That’s when the damage becomes permanent. Lung function drops. Oxygen levels fall. And simple tasks like walking to the mailbox become exhausting.
Why Medications Don’t Cause True Hypersensitivity Pneumonitis
There’s a big difference between drug-induced lung injury and hypersensitivity pneumonitis. Drugs like amiodarone, nitrofurantoin, or chemotherapy agents such as bleomycin can damage the lungs. But they don’t cause the same immune pattern as HP.
True HP shows up under the microscope with:
- Poorly formed granulomas
- Lymphocytes clustering around small airways (bronchiolocentric inflammation)
- Scarring that follows a specific pattern on CT scans
Medication-related lung injury looks different. It might show as organizing pneumonia - where the lung fills with inflammatory tissue - or diffuse alveolar damage, which looks like acute injury from trauma or infection. There are no granulomas. No bronchiolocentric pattern. No history of repeated exposure to airborne antigens.
That’s why experts at the Merck Manual, the Pulmonary Fibrosis Foundation, and major university medical centers don’t list medications as causes of hypersensitivity pneumonitis. They list them under a different category: drug-induced interstitial lung disease (DILD). The names are similar. The symptoms - cough, breathlessness, fatigue - overlap. But the cause, the mechanism, and the treatment are not the same.
What Medications Can Cause Lung Symptoms Like HP?
If you’re on a medication and suddenly develop a dry cough or worsening breathlessness, don’t ignore it. Some drugs are known to harm the lungs:
- Amiodarone (used for heart rhythm problems): Can cause phospholipidosis, leading to scarring over months. Risk increases with higher doses and long-term use.
- Nitrofurantoin (antibiotic for UTIs): Can cause acute pneumonitis within days or chronic fibrosis after months. Often mistaken for pneumonia.
- Bleomycin (chemotherapy): Causes direct toxicity to lung cells. One of the most common drug-related lung injuries in cancer patients.
- Methotrexate (used for rheumatoid arthritis): Can cause acute or subacute interstitial lung disease, especially in older adults or those with existing lung issues.
- Checkpoint inhibitors (immunotherapy drugs like pembrolizumab): Trigger immune attacks on the lungs as a side effect - called immune-mediated pneumonitis.
These reactions aren’t allergic in the way HP is. They’re not triggered by inhaling mold or bird dust. They happen because the drug itself, or your body’s reaction to it, damages lung tissue. The symptoms can be identical: cough, low oxygen, fatigue. But the treatment is different.

How Doctors Tell the Difference
Getting the right diagnosis is critical. Mistaking drug-induced lung injury for HP - or vice versa - can lead to the wrong treatment and worse outcomes.
Here’s how doctors figure it out:
- History: Did you start the medication recently? Are you around birds, mold, or humidifiers? Did your symptoms improve when you traveled away from home?
- Imaging: A high-resolution CT scan shows the pattern. HP has mosaic attenuation and air trapping. Drug injury might show ground-glass opacities without the same air-trapping pattern.
- Blood tests: HP often shows antibodies to specific antigens (like pigeon proteins). Drug reactions don’t.
- Fluid from lungs: Bronchoalveolar lavage in HP shows high lymphocyte counts (>40%). In drug injury, it’s more variable.
- Lung biopsy: The gold standard. If you see granulomas and bronchiolocentric lymphocytes - it’s HP. If you see organizing pneumonia or eosinophils - it’s likely a drug.
One key test: if you stop the medication and your symptoms improve, that’s a strong sign it’s drug-related. If you leave your home or workplace and feel better - that points to HP.
What to Do If You Suspect Lung Trouble from a Drug
If you’re on a medication and notice:
- A new, persistent dry cough
- Shortness of breath that’s worse than usual
- Fatigue that doesn’t go away
- Fever without infection
Don’t wait. Don’t assume it’s just getting older or out of shape. Talk to your doctor. Bring your full medication list - including supplements and over-the-counter drugs.
Early action saves your lungs. Stopping the drug quickly in drug-induced injury can reverse the damage. Waiting too long can lead to permanent scarring, just like in chronic HP.
Doctors may order a chest CT, pulmonary function tests, and blood work. In some cases, they’ll refer you to a pulmonologist who specializes in interstitial lung diseases. These specialists see dozens of these cases every year. They know the subtle differences.
Can You Prevent This?
Yes - but prevention looks different depending on the cause.
For environmental HP:
- Avoid exposure. If you have bird fancier’s lung, rehome the birds or wear a mask and clean cages daily.
- Keep humidifiers, air conditioners, and hot tubs clean. Use distilled water.
- Don’t ignore symptoms. If you feel worse after cleaning the attic or visiting a farm, get checked.
For medication-related lung injury:
- Know your drugs. Ask your doctor: “Can this cause lung problems?”
- Report new symptoms early. Don’t wait for them to become severe.
- Don’t stop medication on your own - but don’t ignore warning signs either.
- Some people are more at risk: older adults, smokers, those with existing lung disease.
There’s no magic test to predict who will react. But awareness saves lives.
What Happens If It’s Not Treated?
Left unchecked, both chronic HP and drug-induced lung injury can lead to pulmonary fibrosis - irreversible scarring that makes your lungs stiff and weak.
Once fibrosis sets in:
- Oxygen levels drop, even at rest
- Walking a few steps becomes hard
- Clubbing of fingers may appear
- Lung transplant becomes the only option
Studies show that 30-50% of people with chronic HP develop fibrosis. The same risk exists with delayed diagnosis of drug-induced injury. The difference? In HP, removing the trigger can stop progression. In drug injury, stopping the drug can reverse it - if caught early.
That’s why timing matters. The sooner you act, the better your lungs will recover.
Final Thoughts
Yes, medications can cause cough and breathlessness. But calling it hypersensitivity pneumonitis is wrong - and misleading. It’s not the same disease. The treatments are different. The prognosis is different.
If you’re experiencing lung symptoms after starting a new drug, get it checked. Don’t assume it’s just a side effect you have to live with. Don’t confuse it with environmental triggers. And don’t wait until you’re gasping for air.
Your lungs are more resilient than you think - but only if you listen to them early.
Can medications cause hypersensitivity pneumonitis?
No, medications do not cause true hypersensitivity pneumonitis. HP is triggered by inhaling environmental antigens like mold, bird proteins, or bacteria. Medications can cause other types of lung injury - called drug-induced interstitial lung disease - but they don’t produce the specific immune response or lung tissue changes seen in HP.
What are the most common drugs that harm the lungs?
Common culprits include amiodarone (for heart rhythm), nitrofurantoin (for urinary tract infections), bleomycin (chemotherapy), methotrexate (for autoimmune diseases), and immune checkpoint inhibitors used in cancer treatment. These drugs can cause inflammation or scarring in the lungs, often mimicking pneumonia or asthma symptoms.
How do I know if my cough is from a medication or something else?
Look at timing. Did the cough start within days or weeks of beginning a new drug? Does it improve after stopping the medication? If your symptoms get worse after being around birds, mold, or humidifiers - and improve when you leave - it’s likely environmental. A doctor can help confirm with imaging, lung function tests, and sometimes a biopsy.
Is hypersensitivity pneumonitis curable?
In its early stages - especially acute HP - yes, it’s often fully reversible if you avoid the trigger. In chronic cases with scarring, the damage is permanent, but progression can be slowed with medications like nintedanib or immunosuppressants. Early diagnosis and strict avoidance of the antigen are key to preventing long-term harm.
Should I stop my medication if I have a cough?
Never stop a prescribed medication without talking to your doctor. But do report new or worsening cough and breathlessness immediately. Your doctor may pause the drug temporarily to see if symptoms improve, order tests, or switch you to a safer alternative. Stopping abruptly can be dangerous - but ignoring symptoms can be worse.
Can I get tested to see if I’m at risk for drug-induced lung injury?
There’s no routine blood test to predict who will develop drug-induced lung injury. Risk factors include older age, existing lung disease, higher drug doses, and longer treatment duration. The best strategy is awareness - knowing which drugs carry lung risks and reporting symptoms early.




Written by Martha Elena
I'm a pharmaceutical research writer focused on drug safety and pharmacology. I support formulary and pharmacovigilance teams with literature reviews and real‑world evidence analyses. In my off-hours, I write evidence-based articles on medication use, disease management, and dietary supplements. My goal is to turn complex research into clear, practical insights for everyday readers.
All posts: Martha Elena