Epigenetic Therapy: What It Is and Why It Matters
If you’ve heard the buzz about "gene‑editing" and wondered why doctors keep talking about "epigenetics," you’re not alone. Epigenetic therapy isn’t about changing the DNA code itself – it’s about flipping the switches that tell genes when to turn on or off. Think of your genome as a library and epigenetic marks as sticky notes that highlight the most important books. When those notes get messed up, cells can go rogue, leading to cancer, autoimmune disorders, or even neuro‑degeneration. Epigenetic drugs aim to clean up those notes so cells behave the way they’re supposed to.
How Epigenetic Therapy Works
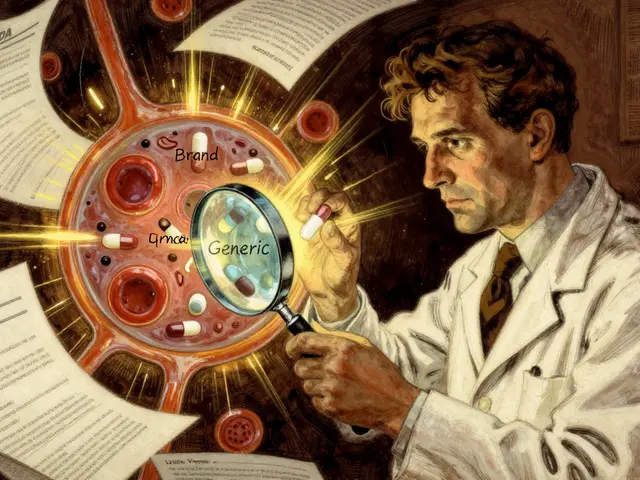
These therapies target the enzymes that add or remove chemical tags on DNA or the proteins that wrap DNA (histones). The most common tags are methyl groups – tiny carbon‑nitrogen pieces that sit on DNA bases and silence genes. Drugs called DNA‑methyltransferase inhibitors (like azacitidine) block the enzyme that puts those methyl groups on, basically telling the cell to read genes that were previously shut down. On the other side, histone‑deacetylase inhibitors (like vorinostat) stop the removal of acetyl groups, keeping the DNA more open and active. By tweaking these processes, doctors can reactivate tumor‑suppressor genes or dampen oncogenes that drive cancer growth.
Common Uses and What Patients Should Know
Right now, epigenetic therapy is mostly used for certain blood cancers, such as myelodysplastic syndromes (MDS) and acute myeloid leukemia (AML). The reason is that these cancers often have a lot of abnormal DNA‑methylation, making them good targets for methyl‑transferase inhibitors. Clinical trials are also testing these drugs for solid tumors, neuro‑degenerative diseases like Alzheimer’s, and even rare genetic disorders where a single gene is turned off incorrectly.
From a patient’s perspective, the side‑effect profile can feel familiar – nausea, fatigue, low blood counts – because many epigenetic drugs affect rapidly dividing cells. The good news is that they’re usually given in cycles, giving the body time to recover between doses. Your oncologist will monitor blood work closely and may adjust the schedule if you experience severe drops in white cells or platelets.
One thing to keep in mind is that epigenetic changes are reversible. That means you might need ongoing treatment to maintain the benefits, especially for chronic conditions. Researchers are also exploring combination approaches – pairing epigenetic drugs with immunotherapy or traditional chemotherapy – to boost overall response rates.
If you’re considering an epigenetic therapy, ask your doctor about the specific drug’s mechanism, how it fits into your overall treatment plan, and what monitoring will look like. Knowing the basics helps you stay informed and makes it easier to weigh the potential benefits against the risks.
Bottom line: epigenetic therapy offers a way to reset faulty gene expression without rewriting the DNA itself. While it’s still a growing field, the early successes in blood cancers give hope that these “gene‑switch” drugs could become a staple for many more diseases in the years ahead.

How Epigenetics Drives Tumor Growth and What It Means for Cancer Treatment
Explore how epigenetic mechanisms like DNA methylation and histone modification fuel tumor growth, affect prognosis, and open new therapeutic doors in cancer care.
Sep 25 2025