PPI-Clopidogrel Interaction Checker
Check Your PPI Safety
When you’re on clopidogrel to prevent heart attacks or stent clots, you might also be prescribed a proton pump inhibitor (PPI) to protect your stomach. It seems logical-take one drug to keep your blood from clotting, another to stop ulcers. But here’s the catch: some PPIs can make clopidogrel less effective. Not all of them. And not always. But when they do, the consequences can be serious.
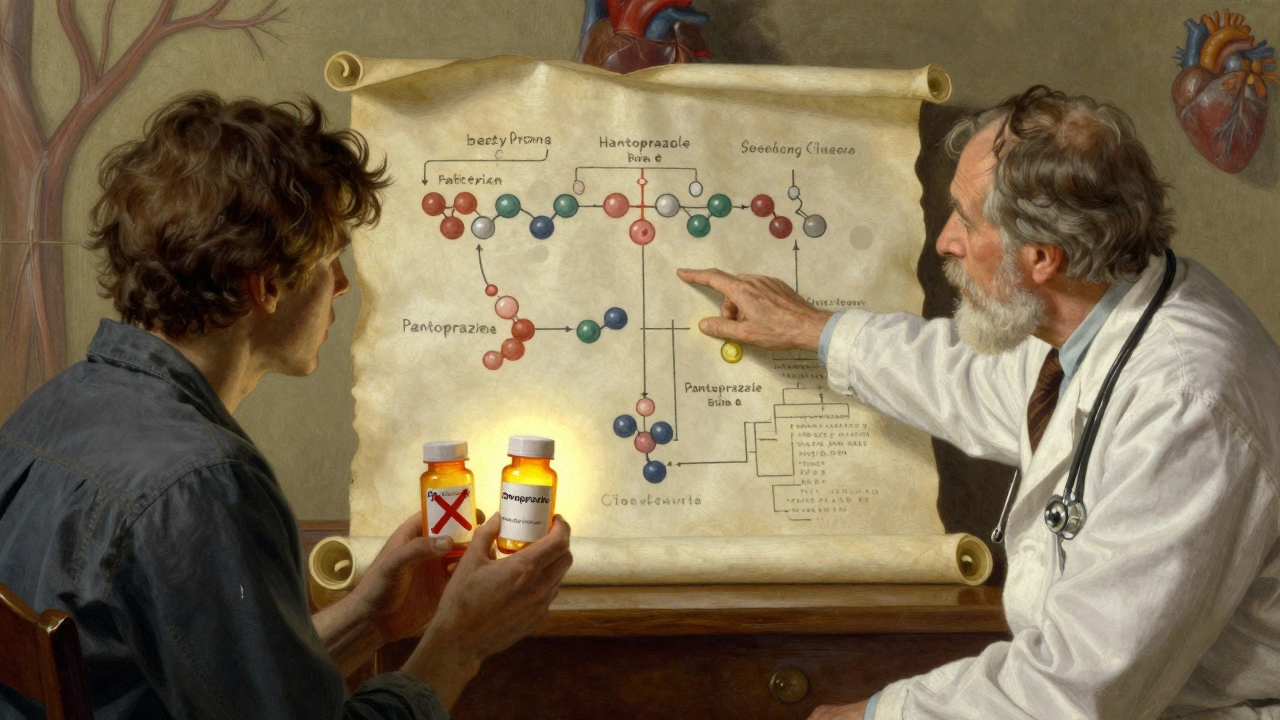
Why Clopidogrel Needs Help to Work
Clopidogrel isn’t active when you swallow it. It’s a pro-drug, meaning your liver has to turn it into something that actually works. That job falls mostly to an enzyme called CYP2C19. If that enzyme is busy or blocked, clopidogrel doesn’t get converted properly. Your platelets stay sticky. Your risk of heart attack or stroke goes up.How PPIs Interfere
PPIs like omeprazole and esomeprazole also rely on CYP2C19 to break down in your body. When you take them together, they fight for the same enzyme. It’s like two people trying to use one printer at the same time-only one gets through clearly. Studies show high-dose omeprazole can slash the active form of clopidogrel by nearly half. Even the standard 20mg dose cuts it by a third.Not All PPIs Are the Same
This isn’t a blanket warning for all acid-reducing drugs. The interaction varies wildly depending on the PPI:- Omeprazole and esomeprazole: Strong inhibitors of CYP2C19. Avoid if possible.
- Lansoprazole: Moderate effect. Use with caution.
- Rabeprazole: Some inhibition, but less consistent.
- Pantoprazole: Minimal effect. The safest choice.
- Dexlansoprazole: Low interaction risk. Also a good alternative.
A 2017 meta-analysis found omeprazole reduced clopidogrel’s effect by almost 39%. Pantoprazole? Barely 4%. That’s not a small difference-it’s the difference between protection and risk.
What the Guidelines Say
In 2023, the American College of Cardiology and American Heart Association updated their advice: if you need a PPI while on clopidogrel, pick pantoprazole or dexlansoprazole. Don’t use omeprazole or esomeprazole. The European Society of Cardiology is even clearer: avoid them entirely.The FDA still has a black box warning on clopidogrel labels about omeprazole and esomeprazole. That’s the strongest warning they give. It’s not just a suggestion-it’s a red flag.
Why Do Doctors Still Prescribe Them?
Here’s where things get messy. Many cardiologists and gastroenterologists disagree on how dangerous this really is. One side says: the data is clear. Patients on omeprazole have higher rates of stent clots and heart attacks. Dr. Deepak Bhatt’s research showed a 53% increase in stent thrombosis.The other side says: in real life, I’ve never seen it happen. Dr. Marc Cohen led the COGENT trial, which found no major spike in heart events-even with omeprazole. He argues that preventing a life-threatening GI bleed is worth the small theoretical risk.
Both sides have data. But here’s what matters: if you’re at high risk for bleeding-over 65, on blood thinners, or have a history of ulcers-you absolutely need a PPI. The question isn’t whether to use one. It’s which one.
Real-World Choices
In hospitals and clinics, the shift is already happening. Since the 2014 FDA warning, prescriptions for omeprazole with clopidogrel dropped by over 24%. Pantoprazole use jumped from 15% to over 42% of co-prescriptions. Why? Because doctors learned the hard way.One internal medicine doctor in Boston reported three cases of stent thrombosis in patients on clopidogrel and omeprazole-all resolved after switching to pantoprazole. That’s not anecdotal. That’s practice-changing.
But cost is a real barrier. Omeprazole costs about $0.38 per pill. Pantoprazole? $1.27. For patients on Medicare or without insurance, that’s a big difference. Some pharmacies still default to omeprazole because it’s cheaper and more familiar.

What Should You Do?
If you’re taking clopidogrel and a PPI, ask these questions:- What PPI am I on? If it’s omeprazole or esomeprazole, ask if you can switch.
- Do I have risk factors for GI bleeding? Age over 65? History of ulcers? On aspirin or warfarin? If yes, you likely still need a PPI-just pick the right one.
- Is there a way to space them out? Some experts suggest taking the PPI in the morning and clopidogrel at night. It’s not perfect, but it might help reduce competition for the enzyme.
- Should I get tested for CYP2C19 gene variants? About 30% of people have genetic variants that make clopidogrel less effective anyway. If you’ve had a stent, heart attack, or clot despite taking clopidogrel, testing might help. It costs $350-$500, but it can guide your treatment.
The Bigger Picture
The future is moving away from clopidogrel altogether. Newer drugs like ticagrelor and prasugrel don’t need CYP2C19 to work. They’re stronger, faster, and don’t interact with PPIs. But they cost over $500 a month. Clopidogrel? Under $5. For millions of people, especially in the U.S., cost matters more than theory.That’s why this interaction won’t disappear. It’s not just science-it’s economics, access, and real-world trade-offs.
What’s New in 2025?
A 2024 study of over 12,000 patients found no link between omeprazole and increased stroke risk. That’s encouraging. But another 2024 study found PPIs may reduce nitric oxide-a molecule that helps blood vessels relax. That could mean PPIs have heart risks beyond clopidogrel.The FDA is reviewing new data from the PEGASUS trial, which showed pantoprazole cut GI bleeding by over half without raising heart risks. That’s the gold standard: protection without trade-offs.
For now, the safest path is clear: if you need both, use pantoprazole. Avoid omeprazole. Talk to your doctor. Don’t stop either drug on your own. But do ask: is this the best combination for me?”
Can I take omeprazole with clopidogrel if I have no other options?
If you’ve tried all other PPIs and still need stomach protection, your doctor may consider omeprazole-but only if you’re closely monitored. Never take it without medical supervision. Some providers may stagger the doses (omeprazole in the morning, clopidogrel at night) to reduce interaction, but this isn’t foolproof. The risk is real, and alternatives like pantoprazole exist for a reason.
Does pantoprazole really work as well as omeprazole for ulcers?
Yes. Multiple studies show pantoprazole is just as effective as omeprazole at healing ulcers and preventing GI bleeding. The only difference is how they interact with clopidogrel. Pantoprazole doesn’t interfere with the enzyme clopidogrel needs, so it’s the safer choice when both drugs are required.
I’m on clopidogrel and feel fine. Do I really need to switch PPIs?
Feeling fine doesn’t mean you’re protected. This interaction doesn’t cause symptoms-it quietly reduces clopidogrel’s ability to prevent clots. You won’t feel a clot forming until it’s too late. If you’re on omeprazole or esomeprazole, switching to pantoprazole is a simple, low-risk move that could prevent a heart attack or stroke.
Are there natural alternatives to PPIs for stomach protection?
No reliable natural alternatives exist for patients on dual antiplatelet therapy. Antacids or H2 blockers like famotidine offer short-term relief but don’t prevent ulcers as effectively as PPIs. For high-risk patients, only PPIs have proven long-term protection. Don’t replace your PPI with supplements or herbal remedies-this could put you at serious risk.
Should I get genetic testing for CYP2C19?
If you’ve had a heart attack, stent, or clot despite taking clopidogrel, testing is worth considering. About 30% of people have gene variants that make clopidogrel less effective. If you’re one of them, switching to a different antiplatelet like ticagrelor may be better than just changing your PPI. The test costs $350-$500, but it can guide life-saving decisions.




Written by Martha Elena
I'm a pharmaceutical research writer focused on drug safety and pharmacology. I support formulary and pharmacovigilance teams with literature reviews and real‑world evidence analyses. In my off-hours, I write evidence-based articles on medication use, disease management, and dietary supplements. My goal is to turn complex research into clear, practical insights for everyday readers.
All posts: Martha Elena