Triptan Medication Interaction Checker
Check Your Medication Safety
Triptans can interact dangerously with certain medications. This tool helps identify potential interactions that could cause serotonin syndrome or other serious complications.
Results
When a migraine hits, people don’t just want relief-they want it fast. Triptans have been the go-to solution for decades, helping millions get back on their feet. But not everyone responds the same way. Some get complete relief. Others feel chest tightness, dizziness, or worse-no effect at all. And if you’re taking other meds, like antidepressants, you might be at risk for something serious. This isn’t just about picking the right pill. It’s about understanding what triptans can and can’t do, who should avoid them, and why they sometimes fail.
What Triptans Actually Do
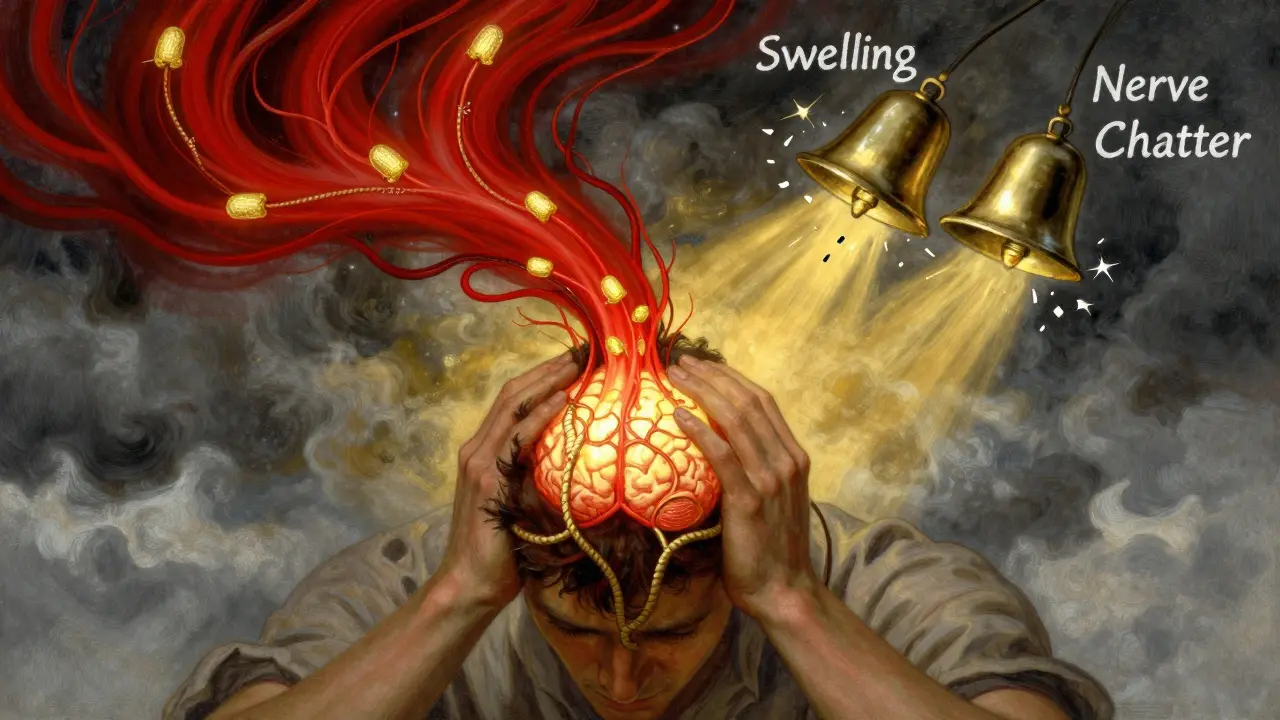
Triptans aren’t painkillers. They don’t numb your brain like ibuprofen or acetaminophen. Instead, they target the root of migraine pain by locking onto serotonin receptors in your head. Specifically, they activate 5-HT1B and 5-HT1D receptors. The 5-HT1B receptor tightens up swollen blood vessels around the brain-something that’s gone wild during a migraine. The 5-HT1D receptor shuts down the release of chemicals like CGRP and substance P, which scream pain signals from your nerves to your brain. Think of it like turning off two alarms at once: one for blood vessel swelling, one for nerve chatter.
That’s why triptans work so well for some people. Studies show that within two hours, between 42% and 76% of users get their headache under control. Around 18% to 50% even feel completely pain-free. That’s better than most over-the-counter options. But it’s not magic. Triptans only work if taken at the right time. If you wait until the pain is screaming, they’re less likely to help. And if you take them during aura-those visual disturbances before the headache-they might even make things worse.
The Seven Triptans You Might Be Prescribed
There are seven FDA-approved triptans, each with subtle differences. They all end in “-triptan,” but their effects vary. Here’s what you need to know:
- Sumatriptan (Imitrex): The original. Works fast, but only 14-15% of it gets into your bloodstream when taken orally. Many people use the nasal spray or injection for quicker results.
- Rizatriptan (Maxalt): Better absorbed-40-45% bioavailability. Often works faster than sumatriptan. Available as a dissolving tablet, which helps if you’re nauseous.
- Zolmitriptan (Zomig): 49% absorbed. Also available as a nasal spray. Good for people who need a middle-ground option.
- Naratriptan (Amerge): Lasts longer. Half-life of 6 hours. Better for migraines that linger, but slower to kick in.
- Frovatriptan (Frova): Longest half-life at 26 hours. Used for menstrual migraines or when attacks last over 72 hours.
- Almotriptan (Axert): Moderate absorption, moderate duration. Often well-tolerated.
- Eletriptan (Relpax): Highest rate of headache relief at two hours-75.3% in studies. But it’s also the most likely to cause side effects like dizziness or fatigue.
One study found that 22% of people had to try at least two different triptans before finding one that worked. Why? Because each one binds slightly differently to receptors. Your body’s chemistry matters more than you think.
When Triptans Don’t Work-And Why
It’s not just about dosage. About 30-40% of migraine sufferers don’t respond to any single triptan. And 20% get zero relief from all of them. That’s not rare. It’s common.
One reason is timing. If you wait more than 20 minutes after the pain starts, the chance of success drops sharply. Migraine isn’t just a headache-it’s a neurological event. The window for triptans to block it is narrow.
Another reason? Cutaneous allodynia. That’s when your skin becomes painfully sensitive-like brushing your hair or wearing glasses hurts. If you have this, triptans lose about half their power. Studies show they’re 70-80% effective in people without skin sensitivity, but only 30-40% effective when it’s present. That’s not a flaw in the drug-it’s a sign your migraine has progressed beyond what triptans can fix.
And then there’s recurrence. Up to 40% of people get their migraine back within 24 hours. Frovatriptan helps here because it lasts longer. But even then, you can’t take a second dose too soon. The rules say at least two hours between doses-and never more than two doses in one day. Break that, and you risk turning occasional migraines into daily ones.

Dangerous Interactions You Can’t Ignore
Triptans aren’t safe to mix with everything. The biggest red flag? SSRIs and SNRIs. These are common antidepressants like fluoxetine (Prozac), sertraline (Zoloft), or venlafaxine (Effexor). Both triptans and these drugs affect serotonin. When combined, they can cause serotonin syndrome-a rare but dangerous condition. Symptoms include confusion, rapid heartbeat, high fever, muscle stiffness, and seizures. It’s not common, but it’s real. And it’s preventable.
Doctors usually don’t stop you from using both, but they’ll watch you closely. If you’re on one of these meds and your migraine suddenly gets worse after taking a triptan, or you feel unusually hot, shaky, or confused-get help immediately.
Another risky combo? Ergotamines. These older migraine drugs are rarely used now, but some people still take them. Mixing ergots with triptans can cause severe, life-threatening blood vessel narrowing. Never take them within 24 hours of each other.
Even something as simple as MAO inhibitors (used for depression or Parkinson’s) can be dangerous. If you’re on one, triptans are off-limits.
Who Should Never Take Triptans
Triptans aren’t for everyone. If you have any of these, avoid them completely:
- History of heart attack or angina
- Coronary artery disease
- Uncontrolled high blood pressure
- Stroke or TIA (mini-stroke)
- Peripheral artery disease
- Severe liver disease
Why? Because triptans constrict blood vessels. If your arteries are already narrowed or damaged, this can trigger a heart attack or stroke. The risk is low-about 0.08 cases per 10,000 people per year with sumatriptan-but it’s real. That’s why doctors screen for heart problems before prescribing.
Even if you don’t have symptoms, if you’re over 40 and have risk factors like smoking, diabetes, or high cholesterol, your doctor might skip triptans and suggest something else.

What Comes After Triptans Fail
When triptans don’t cut it, the next step isn’t more pills-it’s different drugs. Newer options are changing the game.
Gepants like ubrogepant (Ubrelvy) and rimegepant (Nurtec) block CGRP-the very chemical triptans try to shut down. They don’t constrict blood vessels, so they’re safe for people with heart disease. They’re also approved for both acute treatment and prevention.
Ditans like lasmiditan (Reyvow) target a different serotonin receptor (5-HT1F). No vasoconstriction. No heart risk. But they can cause drowsiness, so you can’t drive after taking them.
Some doctors now combine triptans with NSAIDs. The combo of sumatriptan and naproxen (taken together) gives better results than either alone. The pain-free rate jumps from 18% to 27% at two hours.
And for those who get migraines often-15 or more days a month-preventive meds like CGRP monoclonal antibodies (Emgality, Ajovy) are now standard. These are monthly injections that stop migraines before they start.
Real Talk: What Patients Say
Surveys of over 2,500 migraine patients show that 68% found at least one triptan that worked. But 22% had to switch between three or more before finding relief. And 10% didn’t benefit from any.
Side effects are common. About 5-7% feel chest or throat tightness. It’s not a heart attack-it’s a side effect. But it’s scary enough that many stop taking them. Dizziness? Happens in 4-10%. Fatigue? 3-8%. Cost is another factor. Some triptans cost $100 a pill without insurance. That’s why many people abandon them after a year.
One woman in Wellington told her doctor she’d tried four triptans. The first gave her chest pain. The second made her dizzy. The third didn’t help at all. The fourth worked-but only if she took it 15 minutes after the first flicker of light in her vision. She learned to track her aura. Now, she’s migraine-free more often than not.
That’s the truth: triptans aren’t one-size-fits-all. They’re tools. And like any tool, they work best when used correctly, with awareness of limits and risks.
What to Do Next
If you’re on triptans and they’re not working:
- Track your attacks. Note when you take the pill, what time the pain started, and if you had aura.
- Check for skin sensitivity. Does brushing your hair hurt? Is your scalp tender? If yes, triptans may be less effective.
- Review your meds. Are you on an SSRI or SNRI? Talk to your doctor about serotonin risk.
- Don’t push past the 2-dose limit. More isn’t better-it’s dangerous.
- Ask about alternatives. Gepants, ditans, or combination therapy might be better for you.
Migraine treatment isn’t about finding the ‘best’ drug. It’s about finding the right one-for your body, your triggers, and your life. Triptans helped millions. But they’re not the end of the road. They’re just one step.


Written by Martha Elena
I'm a pharmaceutical research writer focused on drug safety and pharmacology. I support formulary and pharmacovigilance teams with literature reviews and real‑world evidence analyses. In my off-hours, I write evidence-based articles on medication use, disease management, and dietary supplements. My goal is to turn complex research into clear, practical insights for everyday readers.
All posts: Martha Elena