When you hear about a new cancer drug hitting the market, it’s easy to think it’s just another pill that works for everyone. But the truth is, biomarkers are now at the heart of who gets to take these drugs-and why. In 2026, nearly every major cancer clinical trial uses specific biological signals to decide who qualifies. This isn’t science fiction. It’s everyday medicine. And if you or someone you know is considering a trial, understanding how biomarkers and inclusion criteria work could make all the difference.
What Are Biomarkers, Really?
Biomarkers are measurable signs in your body that tell doctors something about your health. They’re not just blood tests or scans. They’re specific molecules-like proteins, genes, or mutations-that show whether a cancer is likely to respond to a certain treatment. The FDA defines them as "a characteristic that is objectively measured and evaluated as an indicator of normal biological processes, pathogenic processes, or pharmacologic responses to a therapeutic intervention." In plain terms: if a biomarker is present, the drug might work. If it’s not, the drug probably won’t.
There are seven types of biomarkers used in cancer trials:
- Susceptibility/risk: Shows if you’re more likely to develop cancer (like BRCA1 mutations).
- Diagnostic: Helps confirm you have cancer (like PSA levels in prostate cancer).
- Prognostic: Tells how aggressive your cancer is, regardless of treatment.
- Predictive: The most important one-predicts if a drug will work for you (like HER2 in breast cancer or EGFR in lung cancer).
- Pharmacodynamic/response: Shows if the drug is doing what it’s supposed to do in your body.
- Monitoring: Tracks how your cancer changes over time (like circulating tumor DNA).
- Safety: Flags if you’re at risk for serious side effects.
Today, 73% of oncology trials in 2022 required at least one biomarker for eligibility. That’s up from 41% in 2017. These aren’t optional extras. They’re gatekeepers.
Why Biomarkers Change Everything
Before biomarkers, clinical trials were like throwing a net into the ocean and hoping to catch a fish. Researchers enrolled patients based on cancer type alone-"lung cancer," "breast cancer," etc.-without knowing if the drug actually targeted what was driving each person’s tumor. The result? High failure rates. In the past, over 60% of Phase 2 trials failed because the drug just didn’t work for most people.
Now, trials use biomarkers to filter patients upfront. If a drug targets a specific mutation-say, ALK in non-small cell lung cancer-only patients with that mutation get in. This precision means:
- Trials have a 49.8% success rate in Phase 2, compared to 26.9% without biomarkers.
- Response rates jump dramatically. In one study, using HER2 mutation as an eligibility criterion raised response rates for neratinib from 12% to 32%.
- Patients are less likely to get a drug that won’t help them, reducing unnecessary side effects.
This shift isn’t just about efficiency-it’s about survival. Patients in biomarker-selected trials live longer, on average, than those in older-style trials. And for cancers with few options, like metastatic melanoma or rare sarcomas, this is life-changing.
What Goes Into Inclusion Criteria?
Inclusion criteria are the rules that decide who can join a trial. Biomarkers are now one of the most important rules-but they’re not the only ones. A typical cancer trial might require:
- A confirmed diagnosis of a specific cancer type (e.g., Stage III non-small cell lung cancer).
- A positive test for a specific biomarker (e.g., PD-L1 expression ≥50%, KRAS G12C mutation).
- Measurable disease on a CT or PET scan.
- Good organ function (liver, kidneys, bone marrow).
- No prior treatment with a similar drug.
- Performance status (like ECOG score of 0 or 1)-meaning you’re well enough to tolerate treatment.
These criteria aren’t arbitrary. Each one is based on data. For example, if a drug causes liver toxicity, the trial will only include people with normal liver enzymes. If past trials showed the drug doesn’t work in patients with brain metastases, they’re excluded.
What’s new is how biomarkers are layered into these rules. Instead of just saying "you have lung cancer," the trial now says: "You have lung cancer AND your tumor has a ROS1 fusion gene AND you’ve had one prior chemotherapy." That specificity is what makes modern trials so powerful.

The Hidden Challenges
It sounds perfect, right? But there’s a catch. Getting a biomarker test isn’t as simple as walking into a lab.
First, not every hospital can do the test. Specialized tests-like next-generation sequencing or liquid biopsy-require advanced equipment and trained staff. Many community clinics still can’t offer them. That means patients might need to travel hundreds of miles just to get tested.
Second, turnaround time. A standard blood test gives results in a day. A complex tumor DNA test? It can take 7 to 14 days. During that time, your cancer might be growing. And if the test comes back negative, you’re back to square one.
Third, geographic differences. A biomarker common in Europe might be rare in North America. For example, HLA-A*02:01-a marker used in some cell therapies-is found in 38-53% of Europeans but only 17-48% of North Americans. That means a trial designed for Europe might not work in the U.S., and vice versa.
And then there’s cost. Biomarker testing can run from $1,000 to $5,000. Insurance doesn’t always cover it, especially for experimental trials. Many patients end up paying out of pocket-or skipping the test entirely.
How Trials Are Solving These Problems
The industry knows these issues exist. And they’re trying to fix them.
- Centralized labs: 63% of Phase 3 trials now send all samples to one lab, ensuring consistent testing.
- Standardized kits: 78% of sponsors now send sites pre-packaged collection kits to avoid sample mishandling.
- Liquid biopsies: Blood tests that detect tumor DNA are now used in 31% of Phase 2+ trials-up from just 9% in 2020. They’re faster, less invasive, and can be repeated.
- Real-time data: Some trials now use dashboards that track biomarker results across sites in real time, helping sites adjust enrollment strategies.
- Training: Sites with trained staff enroll patients 28 days faster than those without.
These aren’t just nice-to-haves. They’re making trials faster, fairer, and more effective.
What This Means for You
If you’re considering a clinical trial for cancer, here’s what you need to do:
- Ask if your cancer type has an FDA-approved biomarker test. For example: EGFR, ALK, ROS1 for lung cancer; BRCA for ovarian or breast; MSI-H/dMMR for colorectal.
- Find out if your oncologist can order the test-or if you need to go to a specialized center.
- Ask about turnaround time. If it’s longer than 10 days, ask if a liquid biopsy is an option.
- Check if the trial is part of a network that covers testing costs. Many trials now include biomarker testing as part of the study.
- Don’t assume a negative test means no options. Some trials are now designed for patients without known biomarkers, using combination therapies or immunotherapy.
The goal isn’t just to get into a trial. It’s to get into the right trial. One that matches your biology. That’s the future of cancer care-and it’s already here.
The Bigger Picture
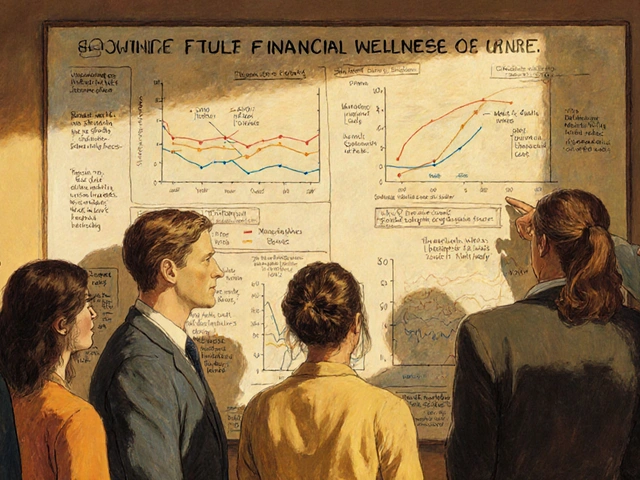
The global biomarker market is growing fast-from $18.7 billion in 2022 to an expected $42.3 billion by 2027. Oncology leads the way, but neurology and immunology are catching up. By 2030, experts predict that 80% of clinical trials will use biomarkers as a core eligibility tool.
This isn’t just about better drugs. It’s about better matching. We’re moving from treating "cancer" to treating "your cancer." And that shift is saving lives.
Do all cancer clinical trials require biomarker testing?
No, not all. But the vast majority of new trials, especially for solid tumors, now do. In 2022, 73% of oncology trials required biomarker testing. Older trials or those testing broad-acting drugs like chemotherapy may still rely on traditional criteria. However, even in those cases, biomarker data is often collected for future analysis.
Can I still join a trial if my biomarker test is negative?
It depends on the trial. Some trials are designed specifically for patients with a certain biomarker and will exclude those without it. Others have "basket" or "umbrella" designs that include multiple subgroups-so even if you’re negative for one marker, you might qualify for another arm. Always ask the research team for details on alternative options.
Are biomarker tests covered by insurance?
In the U.S., many biomarker tests are covered if they’re FDA-approved and used for treatment decisions. However, tests done for clinical trial eligibility are often considered experimental and may not be covered. Many trials now cover testing costs as part of the study protocol. Always ask the trial coordinator before proceeding.
How long does biomarker testing take?
It varies. Simple tests like IHC for PD-L1 can take 3-5 days. Complex genomic tests like whole-exome sequencing can take 2-4 weeks. Liquid biopsies are faster-often 7-10 days. If timing is critical, ask if a rapid testing option is available.
What if I live in a rural area without access to advanced testing?
Many trials now offer mailed sample kits or partner with regional labs to collect and ship tissue or blood. Some use centralized labs that accept samples from anywhere. Ask the trial site if they have a logistics plan for remote patients. You may need to travel once for the test, but follow-up visits can often be done locally.
Can biomarkers change over time?
Yes. Cancer evolves. A biomarker present at diagnosis might disappear after treatment, or new ones might emerge. That’s why some trials now use "dynamic eligibility"-retesting patients during the trial to adjust treatment. Liquid biopsies make this easier, as they can be done repeatedly without invasive procedures.



Written by Martha Elena
I'm a pharmaceutical research writer focused on drug safety and pharmacology. I support formulary and pharmacovigilance teams with literature reviews and real‑world evidence analyses. In my off-hours, I write evidence-based articles on medication use, disease management, and dietary supplements. My goal is to turn complex research into clear, practical insights for everyday readers.
All posts: Martha Elena